Endo-App Übungsmodul
Physiotherapie Aufbaumodul: Beckenboden entspannen
Worum geht es?
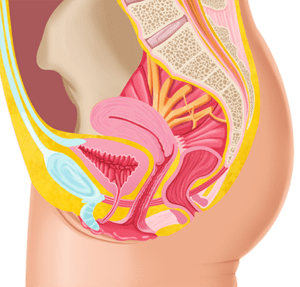
In diesem Modul geht es darum, den Beckenboden zu entspannen. Dass der Beckenboden sich entspannen kann ist wichtig für seine Funktionen, aber vor allem wichtig bei Endometriose da Beckenbodenverspannungen auch Schmerzen machen können.
Modul-Autor:in

Annika Cost – Physiotherapeutin M.Sc.
Wissenschaftliche Grundlagen des Moduls
Annika Cost ist studierte Physiotherapeutin (B.Sc., M.Sc.) und spezialisiert auf Physiotherapie bei Frauen.
Sie ist Mitglied im Deutschen Verband für Physiotherapie und der Global Pelvic Health Alliance.
Allaire C, Williams C, Bodmer-Roy S, Zhu S, Arion K, Ambacher K, Wu J, Yosef A, Wong F, Noga H, Britnell S, Yager H, Bedaiwy MA, Albert AY, Lisonkova S, Yong PJ. Chronic pelvic pain in an interdisciplinary setting: 1-year prospective cohort. Am J Obstet Gynecol. 2018; 218(1):114.e1-114.e12. doi: 10.1016/j.ajog.2017.10.002.
Aredo JV, Heyrana KJ, Karp BI, Shah JP, Stratton P. Relating Chronic Pelvic Pain and Endometriosis to Signs of Sensitization and Myofascial Pain and Dysfunction. Semin Reprod Med. 2017 Jan;35(1):88-97. doi: 10.1055/s-0036-1597123. Epub 2017 Jan 3. PMID: 28049214; PMCID: PMC5585080.
Ball E, Khan KS. Recent advances in understanding and managing chronic pelvic pain in women with special consideration to endometriosis. F1000Res. 2020; 9. doi: 10.12688/f1000research.20750.1.
Berghmans B. Physiotherapy for pelvic pain and female sexual dysfunction: an untapped resource. Int Urogynecol J. 2018; 29(5):631–8. doi: 10.1007/s00192-017-3536-8.
Bordoni B, Zanier E. Anatomic connections of the diaphragm: influence of respiration on the body system. Journal of multidisciplinary healthcare. 2013;6:281–291.
Cameron B, Sabourin J, Sanaee MS, Koenig NA, Lee T, Geoffrion R. Pelvic floor hypertonicity in women with pelvic floor disorders: A case control and risk prediction study. Neurourol Urodyn 2019; 38(2):696–702. doi: 10.1002/nau.23896.
Cottrell MA, Galea OA, O’Leary SP, Hill AJ, Russell TG. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: a systematic review and meta-analysis. Clin Rehabil. 2017; 31(5):625–38. doi: 10.1177/0269215516645148.
Del Forno S, Arena A, Pellizzone V, Lenzi J, Raimondo D, Cocchi L, Paradisi R, Youssef A, Casadio P, Seracchioli R. Assessment of pelvic floor muscles with 3D/4D transperineal ultrasound in women with deep infiltrating endometriosis and superficial dyspareunia treated with pelvic floor muscle physiotherapy: a randomized controlled trial. Ultrasound Obstet Gynecol. 2021. doi: 10.1002/uog.23590.
Findeklee S, Radosa JC, Hamza A, Haj Hamoud B, Iordache I, Sklavounos P, Takacs ZF, Solomayer EF, Radosa M. Treatment algorithm for women with endometriosis in a certified Endometriosis Unit. Minerva Ginecol. 2020; 72(1):43–9. doi: 10.23736/S0026-4784.20.04490-1.
Fuentes-Márquez P, Cabrera-Martos I, Valenza MC. Physiotherapy interventions for patients with chronic pelvic pain: A systematic review of the literature. Physiother Theory Pract. 2019; 35(12):1131–8. doi: 10.1080/09593985.2018.1472687.
Katz L, Fransson A, Patterson L. The development and efficacy of an interdisciplinary chronic pelvic pain program. Can Urol Assoc J. 2020. doi: 10.5489/cuaj.6842.
Klotz SGR, Schön M, Ketels G, Löwe B, Brünahl CA. Physiotherapy management of patients with chronic pelvic pain (CPP): A systematic review. Physiother Theory Pract. 2019; 35(6):516–32. doi: 10.1080/09593985.2018.1455251.
Louw A, Zimney K, Puentedura EJ, Diener I. The efficacy of pain neuroscience education on musculoskeletal pain: A systematic review of the literature. Physiother Theory Pract. 2016; 32(5):332–55. doi: 10.1080/09593985.2016.1194646.
Nijs J, van Paul Wilgen C, van Oosterwijck J, van Ittersum M, Meeus M. How to explain central sensitization to patients with ‚unexplained‘ chronic musculoskeletal pain: practice guidelines. Man Ther. 2011; 16(5):413–8. doi: 10.1016/j.math.2011.04.005.
Nygaard IE, Glowacki C, Saltzman CL. Relationship between foot flexibility and urinary incontinence in nulliparous varsity athletes. Obstet Gynecol. 1996 Jun;87(6):1049-51. doi: 10.1016/0029-7844(96)00079-8.
Piontek K, Ketels G, Albrecht R, Schnurr U, Dybowski C, Brünahl CA, Riegel B, Löwe B. Somatic and psychosocial determinants of symptom severity and quality of life in male and female patients with chronic pelvic pain syndrome. J Psychosom Res. 2019; 120:1–7. doi: 10.1016/j.jpsychores.2019.02.010.
Orr NL, Noga H, Williams C, Allaire C, Bedaiwy MA, Lisonkova S, Smith KB, Yong PJ. Deep Dyspareunia in Endometriosis: Role of the Bladder and Pelvic Floor. J Sex Med. 2018 Aug;15(8):1158-1166. doi: 10.1016/j.jsxm.2018.06.007 . PMID: 30078464.
Sedighimehr N, Manshadi FD, Shokouhi N, Baghban AA. Pelvic musculoskeletal dysfunctions in women with and without chronic pelvic pain. J Bodyw Mov Ther. 2018; 22(1):92–6. doi: 10.1016/j.jbmt.2017.05.001.
Modulinhalte:
- Tag 1: Ort und Funktion
- Tag 2: Warum ist der Bebo verspannt?
- Tag 3: Chronische Schmerzen und der Beckenboden
- Tag 4: Beckenboden entspannen in Rückenlage
- Tag 5: Verschiedene Positionen zum Entspannen
- Tag 6: Triggerpunkte
- Tag 7: Kiefer und Fußgewölbe
- Tag 8: Umliegende Hüft- und Bauchmuskeln