Why is Endometriosis So Often Mistaken for Chlamydia?
You have likely heard of chlamydia, often associated with sexually transmitted diseases. The World Health Organization (WHO) estimates that approximately 89 million new chlamydia infections occur worldwide yearly. In Germany, genital chlamydia infections rank among the most common sexually transmitted pathogens, alongside HPV infections, gonorrhea, and trichomoniasis.
But why does chlamydia capture the interest of the Endo blog? Many individuals with endometriosis report being initially diagnosed with chlamydia before receiving an endometriosis diagnosis. Consequently, in this article, we delve into chlamydia, offering an overview of its symptoms, associated complaints, and potential diagnostic and therapeutic approaches. Given the sometimes challenging differential diagnosis, we also explore similarities with the symptomatology of endometriosis [1], [2], [3].
What Is Chlamydia?
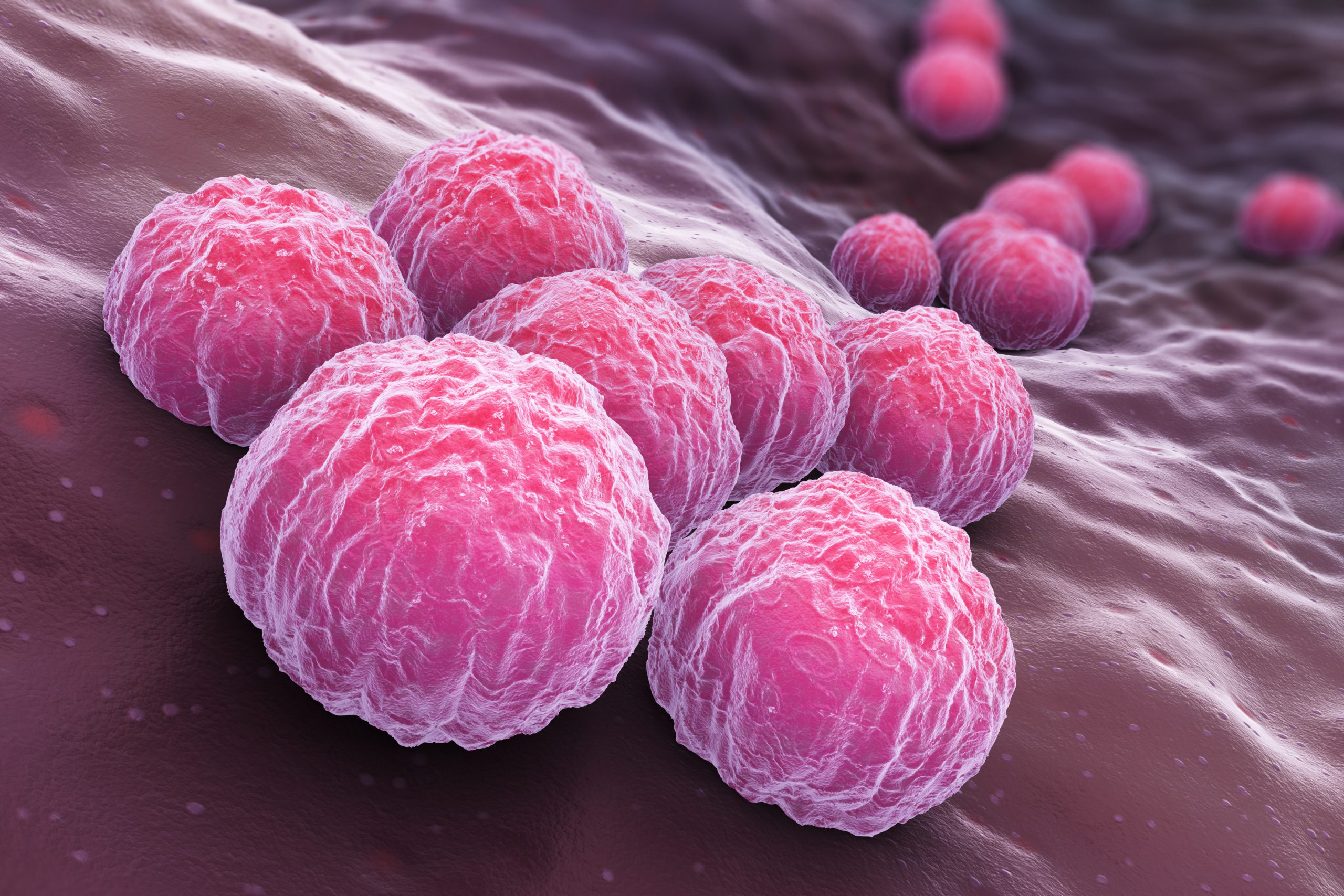
Chlamydia Bacteria
Chlamydia is a type of bacteria capable of causing infections in the human body.
Most chlamydial infections in humans are attributed to two types of pathogens: Chlamydia trachomatis and Chlamydia pneumoniae. Chlamydia trachomatis is responsible for sexually transmitted infections, primarily affecting the genital area, while Chlamydia pneumoniae is associated with respiratory infections like pneumonia and bronchitis [1], [2], [4].
In this article, the primary focus lies on Chlamydia trachomatis, specifically genital chlamydia, which typically leads to inflammation of the urethra, reproductive tract, and rectum. Infection rates vary by region, decrease with age, and many regress with long-term monogamous relationships [1].
How Does Chlamydia Infection Occur?
Infection with the Chlamydia trachomatis pathogen primarily occurs through sexual contact. In most cases, these bacteria are present in the mucous membranes of the rectum, pharynx, vagina, urethra, and cervix. They can also be found in vaginal secretions, semen, the pre-ejaculate fluid, and urine. All sexual activity involving contact with infected mucous membranes or secretions carries the risk of chlamydial infection. This includes vaginal, oral, and anal intercourse. Unprotected vaginal and anal sex are considered the most common modes of transmission. While there is no foolproof method of protection against chlamydia, the use of condoms/femidoms can significantly reduce the risk [1], [2], [4], [8].
What are the Consequences of a Chlamydia Infection?
It is not uncommon for a chlamydia infection to remain asymptomatic, with affected individuals often not experiencing symptoms for some time or with it being undetected through routine medical screening.
Symptoms of chlamydial infection may include the following [1], [4], [5]:
General Symptoms:
- Abdominal pain
- Itching, burning, and/or pain during urination
- Fever
Gender-specific Symptoms:
For Males:
- Burning sensation in the urethra
- White discharge from the penis
For Females:
- Thick, yellowish vaginal discharge
- Intermenstrual bleeding
- Heavy periods
- Pain in the back or abdomen
- Frequent urge to urinate
If left untreated, a chlamydia infection can lead to persistent discomfort and potentially permanent damage, such as chronic pain. Additionally, cervical and rectal infections can occur through oral and anal sex.
In women, chlamydial infection can progress to pelvic inflammatory disease (PID), causing more extensive inflammation of the uterus, fallopian tubes, or ovaries. Unchecked inflammation may damage the reproductive organs, potentially impacting fertility.
Untreated chlamydial infection in men carries the risk of inflammation in the testes, epididymis, and prostate [1], [4].
How is Chlamydia Diagnosed with Certainty?
In many cases, chlamydia infections present with minimal or no symptoms, with approximately 70% percent of infected women and 50% percent of infected men experiencing only mild or no symptoms. Early and accurate diagnosis of chlamydia is crucial to prevent complications and subsequent damage and to enable prompt treatment. Various diagnostic methods are available, the most common being nucleic acid amplification tests and antigen tests [2], [7].
Nucleic acid amplification tests (NAAT) are the most reliable and non-invasive tests for chlamydia diagnosis. During this test, a physician collects a urine sample or a swab from the patient’s cervix or rectum—the test result provides conclusive evidence of the presence of chlamydial DNA in the body.
Antigen tests, while less reliable than NAAT, can still detect chlamydia in the body and are typically conducted using swabs from the cervix or rectum.
Cultures, an outdated diagnostic method for chlamydia, involve obtaining a sample from the affected area and cultivating it on a culture medium. This method is less reliable than NAAT and antigen tests[6], [7].
Individuals at a high risk of infection should undergo regular screening for chlamydia and other sexually transmitted diseases (STIs). This generally includes sexually active women under 25 and individuals with frequent changes in sexual partners. This is because sexually transmitted chlamydia often presents with asymptomatic or nonspecific symptoms, particularly in women, making it likely to go undetected without testing. Routine screening is also recommended for pregnant women. While heterosexual men are not typically screened, homosexual men are advised to undergo screening if they are sexually active. Screening methods include urine tests (for insertive anal sex), rectal swabs (for receptive anal sex), and pharyngeal swabs (for oral sex) [1], [4], [7].
What Are the Treatment Options for Chlamydia?
Individuals affected by chlamydia should not feel ashamed, as it is a common infection that can be effectively treated.

Antibiotics as a treatment for chlamydial infection.
Timely initiation of antibiotic therapy is essential for a speedy recovery, as chlamydia infections can progress quickly. To prevent further transmission, individuals with chlamydia should abstain from sexual intercourse until their treatment is completed. Additionally, it is crucial to note that over 50 percent of the sexual partners of infected individuals are also at risk of infection and should be examined and, if necessary, treated [1], [4], [8].
The most frequently prescribed antibiotic for treating chlamydia in non-pregnant women is doxycycline, taken orally over 7 days. Doxycycline is considered the preferred and first-line treatment. In some instances, macrolide antibiotics such as azithromycin and erythromycin may be prescribed, especially for pregnant women. These antibiotics require a treatment duration of 7 days or longer. Overall, antibiotic treatment yields a success rate of 97 to 100% [4], [7], [11]
What is the Connection Between Chlamydia and Endometriosis? Are There Common Symptoms?
As mentioned earlier, some individuals with endometriosis have reported initially receiving a misdiagnosis of chlamydia before their actual endometriosis diagnosis. How does this misdiagnosis occur?
Both endometriosis and chlamydia infections can present with similar symptoms, although there are distinctions between the symptoms of these two conditions.
Symptoms such as intermittent bleeding, pain during intercourse, discomfort during urination, and infertility can be associated with chlamydia and endometriosis. Given these partially overlapping symptoms, making an accurate differential diagnosis based solely on symptoms can be challenging. Therefore, women experiencing any of them or those at an elevated risk should undergo testing for chlamydia and, if necessary, screening for endometriosis [12].
To clarify, chlamydial infections and endometriosis are distinct medical conditions. Nonetheless, there may be some cases where they are linked. It is hypothesized that inflammation resulting from chlamydial infections might increase the risk of endometriosis by either promoting the growth of endometriosis tissue or impairing the immune response. However, further comprehensive studies and research are required to establish scientifically valid conclusions.
Conclusion
It is crucial to emphasize that not all women with chlamydia infection will go on to develop endometriosis, and having endometriosis does not necessarily imply a chlamydia infection. Nevertheless, when a woman exhibits symptoms of chlamydial infection or is at an elevated risk, undergoing chlamydia testing is advisable. Detecting and treating chlamydia, if present, is essential to minimize the risk of complications, including the development of endometriosis [13], [14], [15], [16].
Referenzen
- German Aids Federation. Chlamydia. https://www.aidshilfe.de/chlamydien#-behandlung-von-chlamydien. Accessed 2 April, 2023.
- Robert Koch Institute. Chlamydioses (part 1): Diseases caused by Chlamydia trachomatis. https://www.rki.de/DE/Content/Infekt/EpidBull/Merkblaetter/Ratgeber_Chlamydiosen_Teil1.html. Accessed 2 April 2023.
- Meyer TF. Max Planck Institute for Infection Biology, Berlin. Federal Ministry of Education and Research. Chlamydia – The underestimated danger. https://www.gesundheitsforschung-bmbf.de/de/chlamydien-die-unterschatzte-gefahr-9257.php. Accessed 2 April, 2023.
- Morris SR. University of California San Diego. MSD Manual. Chlamydial, mycoplasmal, and ureaplasmal mucosal infections.https://www.msdmanuals.com/de-de/profi/infektionskrankheiten/geschlechtskrankheiten/chlamydien-mykoplasmen-und-ureaplasmen-schleimhautinfektionen?query=chlamydien. Accessed 2 April, 2023.
- MSD Manual. Chlamydia. Output for patients. https://www.msdmanuals.com/de-de/heim/kurzinformationen-infektionen/sexuell-übertragbare-infektionen/chlamydien. Accessed 2 April, 2023.
- Gynecologists on the net. Chlamydia. https://www.frauenaerzte-im-netz.de/erkrankungen/chlamydien/diagnostik/. Accessed 2 April, 2023.
- S2k Guideline: Infections with Chlamydia trachomatis (Status: 08/2016)https://www.awmf.org/leitlinien/detail/ll/059-005.html. Accessed 11 April, 2023.
- https://www.netdoktor.de/krankheiten/chlamydien-infektion/. Accessed 4 April, 2023.
- University Hospital Zurich. Chlamydia treatment. https://www.usz.ch/fachbereich/gynaekologie/angebot/chlamydien/. Accessed 4 April, 2023.
- Fertility Center Erlangen. Infertility in women – reasons, diagnosis and treatment.. https://www.kinderwunschzentrum-erlangen.de/unfruchtbarkeit-frau/. Accessed 4 April, 2023.
- Kong FYS, Tabrizi SN, Fairley CK, et al: The efficacy of azithromycin and doxycycline for the treatment of rectal chlamydia infection: a systematic review and meta-analysis. J Antimicrob Chemother 70: 1290–1297, 2015. doi: 10.1093/jac/dku574. Accessed 4 April, 2023.
- Endo App. Knowledge Base. Curious symptoms of endometriosis. https://endometriose.app/kuriose-symptome-bei-endometriose/. Accessed 5 April, 2023.
- Clarizia R, Capezzuoli T, Ceccarello M, et al. Inflammation calls for more: Severe pelvic inflammatory disease with or without endometriosis. Outcomes on 311 laparoscopically treated women. J Gynecol Obstet Hum Reprod (2020). https://www.contemporaryobgyn.net/view/severe-pid-and-without-endometriosis, Accessed 5 April, 2023.
- Takebayashi A, Kimura F, Kishi Y, Ishida M, Takahashi A, Yamanaka A, Takahashi K, Suginami H, Murakami T. The association between endometriosis and chronic endometritis. PLoS One. (2014). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3928198/. Accessed 5 April, 2023.
- Ettore Cicinelli, Giuseppe Trojano, Marcella Mastromauro, Antonella Vimercati, Marco Marinaccio, Paola Carmela Mitola, Leonardo Resta, Dominique de Ziegler, Higher prevalence of chronic endometritis in women with endometriosis: a possible etiopathogenetic link. https://www.sciencedirect.com/science/article/pii/S0015028217303977. Accessed 5 April, 2023.
- Tai FW, Chang CY, Chiang JH, Lin WC, Wan L. Association of Pelvic Inflammatory Disease with Risk of Endometriosis. A Nationwide Cohort Study Involving 141,460 Individuals. J Clin Med (2018): https://pubmed.ncbi.nlm.nih.gov/30352985/. Accessed 5 April, 2023.
Do you have any comments or questions regarding the confusion between endometriosis and chlamydia?
Feel free to leave us a comment.
- Investigating the Effects of Green Tea Complex or Extract on Pain and Mucosal Health - 1. October 2023
- Understanding Primary Dysmenorrhea: Causes, Symptoms, and Treatment - 26. September 2023
- Why is Endometriosis So Often Mistaken for Chlamydia? - 2. September 2023
