Progesterone’s Role in Endometriosis: Unraveling the Impact of a Sex Hormone Gone Astray
In endometriosis, an imbalance in hormone balance becomes evident, with an excess of estrogen and an insufficiency of progesterone being a classic scenario. Additionally, individuals with endometriosis might display progesterone resistance – a situation where the sex hormone does not fully exert its effects, despite being present in ample amounts [1]. However, the significance of the corpus luteum hormone, progesterone, and its relationship with endometriosis remain pivotal inquiries. Today I will furnish you with answers to these intriguing questions and elucidate the role of synthetic luteal hormones in the management of endometriosis.
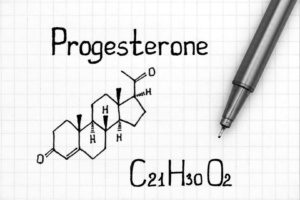
What is Progesterone?
Progesterone, classified as a progestin and often referred to as corpus luteum hormone, takes the reins during the latter half of the menstrual cycle. It is also commonly acknowledged as the pregnancy hormone. A closer look at progesterone’s pivotal functions offers insight into its importance. While the female sex hormone estrogen orchestrates the development of the uterine lining, progesterone steps in afterward to facilitate the implantation of a fertilized egg. Additionally, it prompts uterine growth during pregnancy and lays the groundwork for the upcoming breastfeeding process. Should pregnancy not ensue, the female body experiences a decline in progesterone levels, culminating in menstruation, However, the impact of progesterone is not limited to one domain; it exerts its influence on various organ systems, including blood vessels, intestines, brain, and bones [2].
Progesterone: Tasks Unveiled
Let us delve into a concise overview of progesterone’s functions:
- Preparing the uterine lining, previously built up by estrogen, for successful fertilized egg implantation.
- Eliciting an increase in body temperature during the latter phase of the menstrual cycle.
- Sustaining pregnancy.
- Facilitating mammary gland growth in readiness for breastfeeding [3].
Insufficient Progesterone: Consequences and Detection
Progesterone, predominantly produced in the ovaries, with the placenta joining in during pregnancy, plays a crucial role. Men also produce progesterone, primarily in the adrenal cortex and testes. [4]. This hormone holds significance for male fertility as an intermediate product in hormone metabolism [5].
The pivotal role in progesterone synthesis is triggered by the luteinizing hormone (LH) secreted by the pituitary gland. A stable menstrual cycle hinges on adequate progesterone levels. Insufficiency can lead to cycle disruptions, intermenstrual bleeding, or fertility issues.
Spotting the Signs of Progesterone Deficiency
Symptoms of progesterone deficiency, also termed luteal insufficiency, can be elusive and persist unnoticed. Sometimes, the deficiency is only identified when investigating the cause of infertility.
The following symptoms might emerge due to insufficient progesterone:
- Shortened menstrual cycle, with the second half lasting 12 days or fewer.
- Spotting during the latter part of the cycle.
- Development of growths on the ovaries and uterus (e.g., fibroids).
- Experiencing hot flashes.
- Mood swings and anxiety.
- Disturbed sleep patterns.
- Episodes of dizziness.
- Decreased libido.
- Weight gain attributed to water retention.
Good to know!
Progesterone’s influence on the body is truly remarkable, Its potency becomes particularly evident during pregnancy, a period characterized by elevated progesterone levels. One striking manifestation of its impact is the pronounced pregnancy fatigue, revealing its calming effects on the brain. Furthermore, the hormone’s ability to relax smooth muscle fibers contributes to the occurrence of varicose veins, a not uncommon phenomenon in pregnancy [2].
Endometriosis: Unveiling the Crucial Hormone Cocktail
The functioning of the organism hinges on the intricate orchestration of hormones. This intricate dance is crucial not only for maintaining the female cycle and fostering pregnancy but also for overall well-being. As previously highlighted, progesterone’s ability to induce a sense of tranquility in the brain underscores its potency. The delicate interaction between sex hormones, namely estrogen, and progesterone, holds particular significance in the context of endometriosis. An observable phenomenon within this context is estrogen dominance, where estrogen prevails in abundance over progesterone. This imbalance often extends to endometriosis patients, marked by a dearth of progesterone. In essence, endometriosis can be characterized by an excess of estrogen and a shortage of progesterone. To gain a comprehensive understanding of this hormonal interplay, let’s embark on an exploration into the realm of estrogen—join me on this journey!
Estrogen-Progesterone Exploration
 Estrogen, another essential sex hormone, plays a pivotal role in maintaining a healthy endometrium. Here, estrogen and progesterone collaborate synergistically, facilitated by specialized receptors – dedicated cells or components that receive specific stimuli and transmit them as a signal [6]. However, this is the juncture where endometriosis appears to encounter challenges. Research has indicated disruptions in the estrogen and progesterone signaling pathways with this condition [7]. The implications of malfunctioning signaling pathways extend further, potentially leading to the aforementioned progesterone resistance. Unlike a simple progesterone deficiency, this scenario involves adequate progesterone levels coexisting with receptors that inhibit or obstruct its effects, allowing estrogen to assume a dominant role.
Estrogen, another essential sex hormone, plays a pivotal role in maintaining a healthy endometrium. Here, estrogen and progesterone collaborate synergistically, facilitated by specialized receptors – dedicated cells or components that receive specific stimuli and transmit them as a signal [6]. However, this is the juncture where endometriosis appears to encounter challenges. Research has indicated disruptions in the estrogen and progesterone signaling pathways with this condition [7]. The implications of malfunctioning signaling pathways extend further, potentially leading to the aforementioned progesterone resistance. Unlike a simple progesterone deficiency, this scenario involves adequate progesterone levels coexisting with receptors that inhibit or obstruct its effects, allowing estrogen to assume a dominant role.
Examining Progesterone Receptors
Let’s bear in mind: Evidence suggests that in endometriosis, the signaling pathways governing estrogen and progesterone face disturbances. This disruption can intensify estrogen levels while diminishing progesterone levels. Delving deeper into the subject of progesterone receptors, we uncover their special role in endometriosis. Progesterone acts as the antagonist to estrogen – a balancing force in a healthy cycle. It stimulates the uterine lining’s growth, preparing it for a potential pregnancy. After ovulation, progesterone takes over, maintaining the uterine lining and orchestrating its transformation. This baton-passing analogy is crucial for a well-regulated cycle. Researchers have scrutinized how endometrial cells behave during these phases, revealing that endometriosis cells react less responsively to progesterone, possibly contributing to its emergence [1, 8].
Shifted Dynamics of Progesterone Receptors
Endometriosis tissue does not just appear different; its behavior deviates as well, Let us now delve into these altered dynamics.
Scientific investigations have demonstrated that progesterone’s conventional impact on estrogen is disrupted within endometriosis foci [1, 9]. This phenomenon can be attributed to endometriosis cells’ reduced sensitivity to natural progesterone. Ordinarily, the corpus luteum hormone aids in converting estradiol into estrone via enzymes. This conversion is vital because estrone is significantly less potent. Consequently, progesterone usually mitigates estrogen’s effects. When endometriosis lesions thwart this crucial transformation, it can perpetuate estrogen dominance. The ensuing hormone imbalance fuels inflammation and pain, hallmark features of endometriosis. But the ramifications do not halt there. The density of progesterone receptors also differs within endometriosis tissue. Notably, a particular progesterone receptor (PR-B) is frequently absent. PR-B holds immense importance, as it mediates progesterone’s effects on the endometrium. Normally, progesterone binds to this receptor, triggering a cascade of processes known as progesterone action. With fewer or absent receptors, the cell’s awareness of progesterone is diminished, leading to progesterone resistance. Additionally, fewer representatives of another progesterone receptor (PR-A) are present, which can counteract PR-B effects. Much like hormonal dynamics, the interplay of progesterone receptors is finely tuned and strives for equilibrium [7, 9].
Regulation and Influence of Progesterone Levels
 Further studies yielded a significant discovery—the unresponsiveness of progesterone levels can be attributed to the presence of an increased number of steroid receptors within endometriosis tissue, operating via different regulatory mechanisms [14]. Steroids, a group of hormones synthesized from the basic compound sterane, play a role in producing female sex hormones progestin and estrogen. Another pivotal factor is the abundance of estrogen receptors, which are also elevated within endometriosis tissue. However, not all receptor types experience this increase; for instance, the ERβ receptor type surpasses the ERα receptor type. This is attributed to the fact that ERβ suppresses ERα. This skewed ratio potentially contributes to the heightened detection of estradiol and reduced progesterone [15].
Further studies yielded a significant discovery—the unresponsiveness of progesterone levels can be attributed to the presence of an increased number of steroid receptors within endometriosis tissue, operating via different regulatory mechanisms [14]. Steroids, a group of hormones synthesized from the basic compound sterane, play a role in producing female sex hormones progestin and estrogen. Another pivotal factor is the abundance of estrogen receptors, which are also elevated within endometriosis tissue. However, not all receptor types experience this increase; for instance, the ERβ receptor type surpasses the ERα receptor type. This is attributed to the fact that ERβ suppresses ERα. This skewed ratio potentially contributes to the heightened detection of estradiol and reduced progesterone [15].
In essence, the exploration of hormone-receptor interactions on cellular surfaces continues, shedding light on the changes within this intricate framework.
Gut zu wissen!
Du möchtest mehr über Östrogen und über die Verbindung mit Endometriose erfahren? Dann empfehle ich Dir unseren Artikel: Östrogen und Endometriose: spannende Zusammenhänge.
How is a Progesterone Imbalance Treated?
Numerous studies substantiate longstanding suspicions held by experts: Both the quantity of progesterone and its effectiveness via receptors play pivotal roles in the development and treatment of endometriosis. Reduced progesterone levels and progesterone resistance (diminished signal transmission to cells) can lead to decreased efficacy.

Addressing this hormonal imbalance involving the corpus luteum hormone and estrogen involves the use of synthetic progestins. These are artificially produced corpus luteum hormones that can emulate the effects of the body’s natural progesterone. Progesterone receptors respond to synthetic progestins, often yielding an anti-estrogenic impact.
The list of synthetic progestins is extensive, encompassing:
- Dienogest
- Chlormadinone
- Cyproterone
- Desogestrel
- Drospirenone
- Dydrogesterone
- Etonogestrel
- Gestodene
- Levonorgestrel
- Medrogestone
- Medroxyprogesterone
- Megestrol
- Nomegestrol
- Norethisterone
- Norgestimate
- Norelgestromin
- Tibolone
- Trimegeston
Not every synthetic progestin is equally suitable
The diversity of available options doesn’t imply uniform suitability for endometriosis treatment. The German Society for Gynecology and Obstetrics guideline program recommends employing progestin as the primary agent in symptomatic drug therapy. Dienogest, for instance, is recommended for this purpose. Synthetic progestins can positively influence the size of the endometriosis lesions and mitigate the risk of recurrence post-surgical removal.
However, the nature and location of the endometriosis lesions are determining factors. Dienogest, in particular, exhibits promise due to its demonstrated efficacy in reducing lesion size. Nonetheless, individual suitability hinges on the evaluation of progesterone and estrogen receptors, which vary based on the type of endometriosis present – whether rectovaginal or peritoneal [1, 12].
Considering Potential Side Effects
If your doctor has prescribed progesterone-based medication, they intend to alleviate pain and other symptoms. However, like with any medication, side effects cannot be entirely ruled out. Intermittent bleeding, mood swings, and reduced libido might occur. In the event of unwanted side effects, consulting your doctor is advised. They can assess whether an alternative medication might better suit your needs [13].
Good to know!
Effective endometriosis treatment is a collaborative effort between you and your treating physician. The consideration of your individual circumstances is paramount. Factors such as the extent of endometriosis, its location, and your symptoms all play a crucial role. Ideally, the treatment’s progression is consistently monitored and adapted when required. It is worth noting that if your aim is to conceive, progesterone treatment might not be a suitable option, as progestins and progesterone derivatives constitute the active ingredients in birth control pills.
Short and to the Point
The presence and progression of endometriosis are intricately tied to the hormonal milieu within your body. Amidst the array of hormonal players, both estrogen and progesterone emerge as key protagonists. The corpus luteum hormone, progesterone, assumes the role of estrogen’s antagonist, ushering endometriosis cells into a quiescent phase, Intriguingly, scientific inquiry has highlighted the potential for a hormonal imbalance within endometriosis. Typically, an abundance of estrogen and a scarcity of progesterone are observed. Research has illuminated variations in the behavior of progesterone receptors within individuals with endometriosis. Firstly, these receptors appear to be present in diminished quantities, rendering the available progesterone less potent. Secondly, these receptors demonstrate reduced efficacy in converting estradiol to estrone. Altered regulatory mechanisms within steroid receptors, coupled with an estradiol receptor imbalance, further contribute to the intricate hormonal landscape. These substantial alterations foster a hormonal imbalance—excessive estrogen’s influence can, in turn, bolster inflammation and pain development. In a bid to restore equilibrium, synthetic progestins step onto the stage. However, it is crucial to approach hormone therapy in tandem with your physician. This collaborative approach ensures that hormone therapy aligns with your individual context, and the selection of an appropriate preparation is paramount.
References
- Endometriosis, current drug therapy recommendations with emphasis on hormonal therapy with progestins
- Progesterone – more than a pregnancy hormone – TRIAS Verlag – Gesundheit (thieme.de)
- Progesterone – hormones – women’s cycle | Health Portal
- Progesteron – DocCheck Flexikon
- Progesterone formation in men (hormonspezialisten.de)
- receptors | healthinformation.org
- Marquardt RM, Kim TH, Shin JH, Jeong JW. Progesterone and estrogen signaling in the endometrium: what goes wrong in endometriosis? Int J Mol Sci. 2019 Aug 5;20(15):3822. doi: 10.3390/ijms20153822. PMID: 31387263; PMCID: PMC6695957.
- Female hormones ” About estrogen, progesterone & co. | minimed.at.
- Bulun SE. Endometriosis. N Engl J Med. 2009 Jan 15;360(3):268-79. doi: 10.1056/NEJMra0804690. PMID: 19144942.
- 015/045 – Diagnosis and treatment of endometriosis (awmf.org).
- Angioni S, Pontis A, Malune ME, Cela V, Luisi S, Litta P, Vignali M, Nappi L. Is dienogest the best medical treatment for ovarian endometriomas? Results of a multicentric case control study. Gynecol Endocrinol. 2020 Jan;36(1):84-86. doi: 10.1080/09513590.2019.1640674. epub 2019 Jul 16. PMID: 31311360.
- Götze F (2014) Endometriosis and pelvic pain. St. Gallen Pelvic Floor Symposium.
- Treatment options for endometriosis (gesundheitsinformation.de).
- Pharmaceutical Companies and Their Influence on Scientific Research - 7. October 2023
- Identification of a Genetic Factor Linked to Endometriosis Development and Potential Therapeutic Targets - 6. October 2023
- Identification of a Genetic Factor Linked to Endometriosis Development and Potential Therapeutic Targets - 6. October 2023
