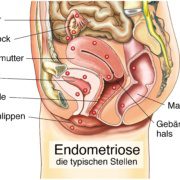
Multimodal Pain Therapy for Endometriosis

Multimodal pain management is an important component of endometriosis therapy
Multimodal pain therapy for endometriosis unfortunately remains relatively underemphasized. Due to delayed diagnosis or recurrence, women with endometriosis face a heightened risk of developing chronic pain. It’s common for this pain to persist independently of the presence of endometriosis. As a result, surgical intervention often proves insufficient for effective pain management, necessitating the addition of multimodal pain therapy.
Multimodal pain management encompasses diverse treatment strategies, integrating medical, dietary, psychological, and physiotherapeutic elements. This approach capitalizes on the potential impact that exercise, mental well-being, nutrition, and other factors can have on mitigating pain.
Especially in cases of persistent and challenging symptoms, the implementation of this comprehensive treatment program as an intensive therapy often yields meaningful outcomes.
Multimodal therapy entails a range of treatment modalities meticulously tailored to the specific condition.
Why is Multimodal Pain Management Important?
Women who endure the challenges of endometriosis often bear a protracted journey of suffering. All too frequently, it takes several years before the underlying cause of their symptoms is identified and a diagnosis is finally reached. Consequently, these years pass with either no therapy or limited interventions.
As a result, many experience chronic pain by the time a diagnosis is established. Furthermore, even in cases of early diagnosis, the recurrence rate remains remarkably high. Thus, at every stage of the journey, preventing the transition to chronic pain stands as a paramount treatment objective, not only for healthcare providers but especially for the affected women themselves.
Additionally, some women afflicted by endometriosis also develop psychosomatic symptoms and are predisposed to depression due to the substantial decline in their quality of life. When pain inhibits participation in social activities and even intimate relationships become impossible, partnerships are also placed under strain.

A team against pain – multimodal pain therapy involves many disciplines!
In many instances, relying solely on drug or surgical interventions falls short of effectively alleviating the patient’s symptoms. This is where the role of multimodal pain therapy for endometriosis becomes vital. To ensure the most effective treatment and sustainable pain relief, a personalized treatment plan must be developed.
The primary objective of multimodal pain therapy goes beyond mere pain relief; it encompasses empowering patients with strategies to influence their pain and enhance their self-efficacy. A critical aspect is the incorporation of numerous measures over the long term.
Multimodal pain therapy for endometriosis typically spans several weeks and can be administered on both an outpatient and inpatient basis within specialized pain therapy centers. Subsequently, it is essential to seamlessly integrate various behavioral changes into daily life to attain optimal outcomes.
Proven Effectiveness in Diverse Chronic Pain Domains
Chronic pain stemming from endometriosis frequently persists for extended periods, potentially leading to enduring psychological distress and subsequent health complications. The profound negative impact on the quality of life among affected women can even curtail their ability to engage fully in routine social interactions.
Hence, beyond medical interventions targeting endometriosis itself, it becomes imperative to incorporate physical and psychotherapeutic interventions.
What Areas does Multimodal Pain Management Cover?
Grasping the Nature of Chronic Pain
Imparting patients with thorough education and insights into the origins of their pain constitutes a pivotal facet of multimodal pain management. Empowering individuals with an understanding of the precise factors underlying their pain equips them with tools to better address the symptoms on their own terms. Moreover, recognizing that physiological underpinnings exist for the pain is crucial; multimodal pain therapy staunchly avoids dismissing pain as merely a figment of the imagination.
Grasping the Complexity of the Condition
Endometriosis is a multifaceted ailment. Gaining a comprehensive understanding of the condition and being able to categorize its impact on one’s own life fosters acceptance and a solution-focused approach. This, in turn, contributes to more favorable outcomes in therapy.
Psychological Intervention
The psychological toll imposed by endometriosis can be substantial, underscoring the relevance of integrating psychological strategies into modular therapy. Practices like mindfulness meditation, for instance, can exert a significant positive influence on psychological well-being.
Physiotherapy
Physiotherapy can serve as a pivotal tool for alleviating not only endometriosis-related pain, but also addressing issues like organ dysfunction and bladder weakness.
Meditation
Engaging in mindfulness exercises and meditation yields profound relaxation while fostering enhanced concentration. This practice proves effective in easing both acute and chronic pain. Additionally, techniques like autogenic training and hypnosis can offer valuable contributions to pain management.
Medication
The conventional approach to pain management involves medication. Nonetheless, medication in isolation often falls short in addressing chronic pain comprehensively. Nevertheless, skillful utilization of pain relievers, particularly during the initial stages, in conjunction with multimodal pain therapy can yield pain relief. This approach proves particularly valuable for managing acute discomfort, such as post-operative pain, to deter the onset of chronic pain.
Acupuncture
Acupuncture, an integral facet of traditional Chinese medicine, is progressively being integrated into chronic pain management. It can also serve as a beneficial complement for individuals grappling with endometriosis.
By strategically placing needles at specific acupuncture points, practitioners aim to diminish the severity and duration of pain.
Exercise therapy
The discomfort arising from endometriosis frequently extends to various regions of the body. Consequently, the resultant compromised posture can exert stress on the spine, joints, and lower limbs. In this context, exercise therapy can yield favorable outcomes. Engaging in physical activity also bestows psychological benefits, enhancing mood and bolstering resilience against challenges. Moreover, exercise can act as a countermeasure against depression.
Muscular Strengthening
Focused muscle building holds equal importance in managing chronic pain, complementing exercise efforts. Given that endometriosis often prompts an instinctive protective posture, strengthening the muscles in the back becomes particularly crucial.
Osteopathy
Osteopathy is dedicated to resolving bodily blockages and harnessing the body’s innate self-healing capacities. Through manual interventions, this practice addresses functional disruptions and, consequently, pain.
Promisingly, initial studies already indicate the efficacy of osteopathy in alleviating endometriosis-related symptoms.
Massage
Massage therapy has established its effectiveness in managing chronic pain. By inducing muscle relaxation, massages offer respite and relief from discomfort.
Nutrition
Diet plays a dual role in influencing pain, with potential positive and negative effects. A study exploring the relationship between diet and endometriosis unveiled a noteworthy connection between specific food consumption and susceptibility to endometriosis.
Neurosacral Modulation
Sacral neuromodulation has already solidified its status as a therapy for select chronic pain disorders. In the realm of endometriosis, preliminary pilot studies have yielded encouraging outcomes.
This innovative approach employs implanted probes to administer subtle electronic impulses, shaping pain perception. Currently under investigation, its application is limited to cases of stubborn pain due to its invasive nature.
Record Keeping and Pain Diary
Maintaining meticulous records is equally crucial. Those who conscientiously document symptoms and interventions are better poised to discern patterns, expediting the identification of effective strategies. Whether through a physical journal, an Excel spreadsheet, or our dedicated app with concise analyses, this practice enhances the integration of helpful measures into daily routines.
Tailored Therapeutic Approaches
From the soothing embrace of a hot water bottle to customized exercises, yoga, and even creative therapy, the aim is to pinpoint what uniquely alleviates individual pain. While self-discovery may not offer a cure for endometriosis, it undoubtedly enhances long-term quality of life, rendering the journey with it significantly more gratifying.
References
What has been your experience with Multimodal Pain Management?
Feel free to leave us a comment.
- Current Research on Endometriosis: An Interview with Deborah Bush - 6. February 2024
- Pain and Pain Management – Interview with Rehab Psychologist Teresa - 19. November 2023
- Physiotherapy for Endometriosis – Interview with Annika Cost – with Exercises - 19. November 2023