The Connection Between Endometriosis and Gut Microbiome
A robust and healthy gut microbiome influences our overall health and bodily functions more than one might imagine. Consequently, it stands to reason that any alterations can yield unexpected negative consequences. Maintaining a healthy intestinal flora is particularly important in the context of endometriosis, as the microbiome, encompassing all microorganisms inhabiting the intestines, regulates hormone balance.
The Gut Microbiome: A Vital Component of the Immune System
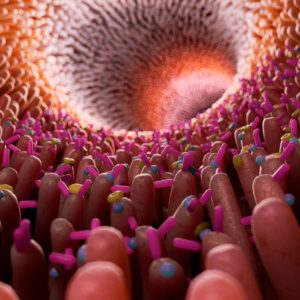
A robust and balanced gut microbiome is pivotal in maintaining overall health. The intestines constitute the most significant component of the human immune system. Over 10^14 microorganisms (one followed by 14 zeros) coexist inside the human gut. Remarkably, each individual possesses their unique “gut microbiome fingerprint,” comprised of approximately 800 to 1000 distinct microorganisms.
Delving deeper into the intricacies of the gut and its functions reveals the importance of minimizing disruptions to our body’s natural intestinal “ecosystem.” Even in healthy individuals, dietary modifications, stress, prebiotics, and antibiotics can induce alterations in the gut microbiome. Researchers have identified changes in the intestinal flora in connection with various conditions, including endometriosis.
Consequences of a Disrupted Gut Microbiome
When the gut microbiome experiences alterations or damage, its ability to perform its essential functions becomes compromised. This can disrupt digestion and hinder the absorption of essential nutrients like vitamins, carbohydrates, amino acids, and minerals. Consequently, these disruptions may lead to various consequences, such as:
- Impaired wound healing
- Hair loss
- Mood swings
- Skin issues like angular cheilitis and other dermatological problems
- Anemia
Animal studies have shown that the gut microbiome can even impact mood. In one experiment, mice with germ-free intestines were given the gut microbiota from particularly anxious animals, transforming them from “normal mice” into “anxious mice.” Conversely, transferring the appropriate gut microbiota could make anxious mice more courageous. While the extent to which these findings apply to humans is not yet entirely clear, initial results strongly suggest that disruptions in the gut microbiome may also contribute to conditions like depression in humans.
The Interplay Between Endometriosis and Gut Microbiota
A comprehensive meta-study scrutinized findings from 18 scientific investigations to probe the relationship between endometriosis and the gut microbiota. The results revealed a discernible difference in the intestinal flora of individuals with endometriosis compared to their healthy counterparts.
Acknowledging that the association between endometriosis and altered gut microbiota is bidirectional is crucial. An imbalanced intestinal flora can exacerbate endometriosis, but it may precipitate changes in the gut microbiota due to potential alterations in the intestinal mucosa. In essence, gut flora influences endometriosis, and endometriosis, in turn, affects gut flora. But how does this intricate interplay manifest?
The microbiome actively participates in the synthesis of various hormones, including estrogen. When the intestinal flora experiences disruption, it inevitably impacts hormone regulation. In the case of endometriosis, the altered microbiome contributes to elevated estrogen levels. High estrogen levels function as a growth stimulus for endometriosis lesions, implying that disturbed gut flora can foster the development of endometriosis.
Endometriosis is characterized by inflammatory processes, and here, too, the gut microbiota exerts influence. When the microbiome is perturbed, it can promote the proliferation of “inappropriate” intestinal bacteria that exacerbate inflammatory responses. Thus, a healthy gut microbiome is pivotal in mitigating inflammatory processes.
Given that the intestines constitute a significant portion of the human immune system, it is paramount to maintain a healthy gut flora to bolster immune functions. A weakened immune system can exacerbate the symptoms of endometriosis.
Lastly, as mentioned earlier, a balanced gut microbiome contributes to sound mental health and robust digestion. In summation, for individuals grappling with endometriosis, nurturing a diverse and healthy gut microbiome through dietary choices can:
- Stabilize estrogen levels
- Alleviate inflammation
- Bolster mental well-being
- Regulate digestion
- Enhance immune resilience
Since endometriosis and gut flora are interdependent, it underscores the importance of fostering a naturally robust microbiome through dietary interventions.
Enhancing Gut Microbiota Through Nutrition
An intestine-healthy diet not only fortifies the gut microbiota but can also aid in alleviating and preventing various complaints. It is important to emphasize that a diet conducive to healthy gut flora is not synonymous with prebiotics in tablet form or indulging in costly specialty products containing specific strains of lactic acid bacteria. Gut-healthy nutrition is not about “functional food” but revolves around a balanced, wholesome diet. The following dietary components play a pivotal role in fostering the development and maintenance of a robust, healthy gut flora:
Dietary fiber:
Dietary fiber is a vital cornerstone of gut-healthy nutrition by nourishing the healthy intestinal flora. Fruits, vegetables, and whole-grain products are rich sources of dietary fiber. However, it is crucial to gradually approach fiber intake if your diet is predominantly low in fiber.

Sudden high fiber intake may overwhelm an undernourished intestinal flora, potentially leading to digestive issues. Slowly increase fiber consumption to avoid this, allowing your intestines to adapt over time. Incorporate whole-grain flour-based products into your diet, including bread, cookies, cakes, pasta, and cereals. Additionally, opt for whole-grain rice over refined white rice. Whole-grain products offer long-lasting satiety, helping curb cravings and support overall gut health.
Lactic Acid Bacteria:
Supporting a robust intestinal flora with lactic acid bacteria does not necessitate the purchase of costly probiotic milk products or supplement pills that tout health benefits in advertisements. It is essential to adopt a critical stance toward dietary supplements. Read more about this in our article on Dietary Supplements for Endometriosis.
A diverse array of lactic acid bacteria from various foods is just as effective and budget-friendly. Low-fat natural yogurt, sour cream, soured milk, raw sauerkraut, sour cucumbers, kimchi, and vegan dairy products all contain lactic acid bacteria. Fermented beverages like bread drinks, sauerkraut juice, kefir, ayran, and drinking yogurt are also sources of these beneficial bacteria, but ensure they are sugar-free.
Avoid Alcohol:
Even minimal alcohol consumption can adversely affect intestinal cells and the gut microbiota. Some studies suggest a potential link between alcohol consumption and an increased risk of endometriosis, although further research is needed for conclusive findings. Regardless, alcohol is a cell toxin that should be consumed sparingly for overall health, irrespective of endometriosis or gut flora considerations.
Low Sugar:
Research indicates that high sugar consumption can promote intestinal bacteria associated with inflammation, a significant concern in endometriosis. While ongoing research aims to establish a definitive link between dietary sugar and its effects on endometriosis, it is advisable to minimize sugar intake. Sugar tends to favor the proliferation of undesirable gut bacteria. Therefore, a sugar-free diet is prudent, as sugar’s detrimental effects extend beyond its potential association with endometriosis.

In summary, a diet that nurtures a healthy intestinal flora is
primarily plant-based, abundant in dietary fiber derived from fruits, vegetables, and whole-grain products, devoid of sugar, rich in diverse lactic acid bacteria, and free from alcohol. Such a diet promotes a thriving gut microbiome, inhibits endometriosis lesions’ growth, alleviates inflammation, strengthens the immune system and psychological well-being, and regulates digestion.
References
- The Gut Microbiota and Inflammation: An Overview – PubMed (nih.gov)
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5564533/
- High Intake of Sugar and the Balance between Pro- and Anti-Inflammatory Gut Bacteria (nih.gov)
- Potential involvement of the immune system in the development of endometriosis (nih.gov)
- Rehab for endometriosis – Interview with rehab psychologist Teresa Götz - 15. March 2024
- Interview with Silke Neumann about Superfoods - 19. November 2023
- Interview with Silke Neumann about Healthy Sugar Alternatives - 18. November 2023