Psychoneuroimmunology – Immune System in Permanent Stress
It is widely recognized that maintaining a healthy diet, getting adequate sleep, and engaging in regular exercise benefit our bodies and immune systems. However, were you aware that our emotions and feelings can significantly influence it, too?
This phenomenon falls under the umbrella of psychoneuroimmunology (PNI). This article will delve into what it entails and explore its relevance to endometriosis.
A Brief Explanation of Psychoneuroimmunology
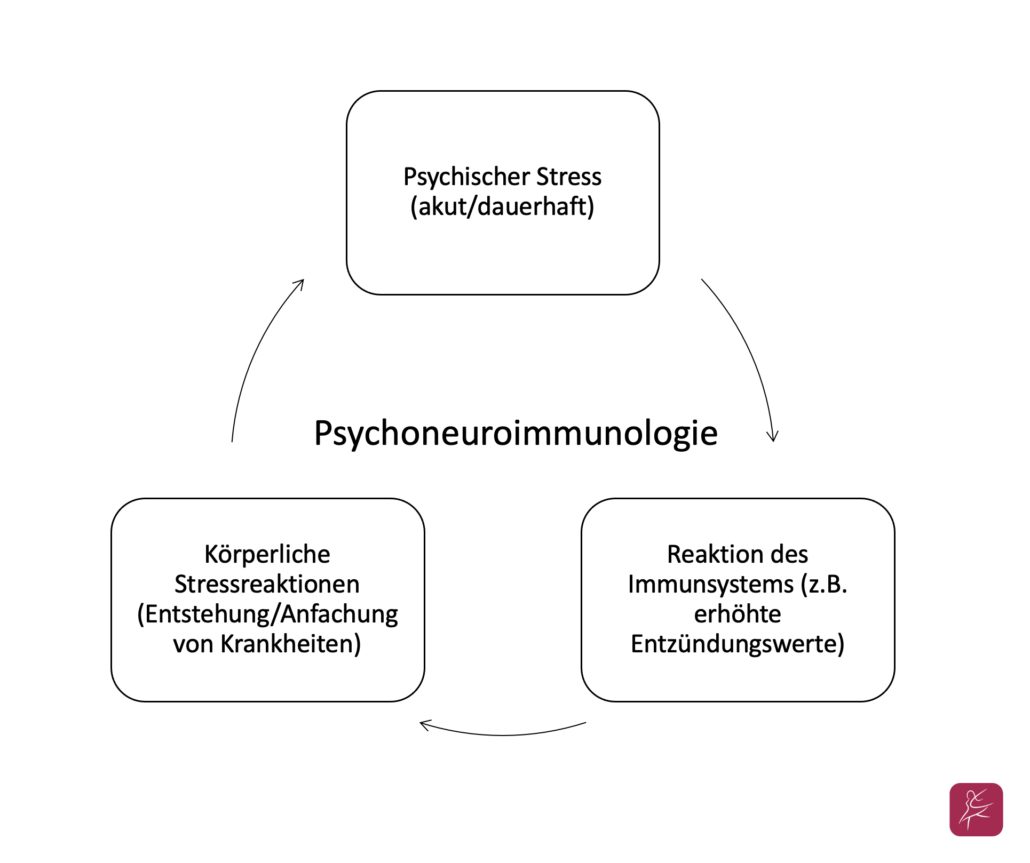
The underlying concept of this tongue twister is relatively straightforward: our body and mind are intricately connected, and emotions like stress or fear can exert a direct and adverse impact on our immune system. There was once a prevailing belief that our immune system operates independently, functions independently, and resists external influences. However, this perspective is now considered outdated. Instead, we understand that the nervous, hormonal, and immune systems are profoundly intertwined, communicating through a shared biochemical network [1].
There are two distinct types of stress: psychological stress, which can stem from issues like relationship problems or workplace anger, and physical stress, resulting from injuries, burns, or general illnesses. Research indicates that individuals exposed to psychological stress often concurrently experience increased inflammatory markers within their bodies. Similarly, physical stressors trigger very similar bodily responses.
It is also crucial to differentiate between acute and chronic stress, whether psychological or physical. Acute stress temporarily ramps the immune system, with natural defense cells becoming active. A brief spike in inflammatory activity enhances the body’s ability to combat invading pathogens. However, if this heightened state persists for an extended period or occurs regularly, the body fails to return to its resting state. Inflammation persists, a condition known as silent inflammation, and psychological or physical stress becomes chronic. This situation is especially critical when the body is already on high alert, such as during an illness, leading to an immune system crash [2]. In this state, the body becomes significantly more susceptible to infections, like respiratory diseases [3], and it also creates a favorable environment for the development and spread of tumors [1].
So, how does all of this relate to endometriosis?
Hormones, stress, and inflammation frequently arise in discussions about endometriosis. It is evident that symptoms, such as persistent pain and even infertility, are closely linked to physical and psychological stress. A study examining the connection between endometriosis and psychoneuroimmunology (PNI) discovered that individuals with endometriosis often exhibited significantly heightened levels of inflammation and increased immune cell activity, which are clear indicators of a psychoneuroimmunological response [4].
Another intriguing aspect is the correlation between PNI and autoimmune diseases. While endometriosis is not classified as an autoimmune disease, it is associated with various autoimmune syndromes [5]. In the field of PNI, researchers are exploring how stress influences the development of such conditions. The elevated and sustained inflammatory activity resulting from psychological and physical stress could explain these connections.
The stress hormones adrenaline, noradrenaline, and cortisol are vital in helping us effectively deal with stressful situations. These hormones have a long history dating back thousands of years. Even our ancestors, when facing formidable threats like the notorious saber-toothed tiger, relied on adrenaline, noradrenaline, and cortisol to bolster their chances of survival. Thanks to evolution, remnants of this mechanism persist in our physiology.
Breaking the Cycle of Chronic Stress
The encouraging news is that you can take proactive steps to combat chronic stress and its associated consequences. The primary target for intervention is often the psychological component of psychoneuroimmunology (PNI), as it is an area where we can exert significant influence. Relaxation techniques provide one practical approach. While they may require some practice, they can yield substantial benefits when incorporated into your routine. Additionally, they play a pivotal role in multimodal pain therapy. These techniques help alleviate chronic stress and address the pain associated with endometriosis.
If you suspect that the root cause of your stress runs deeper, psychosomatic psychotherapy may also be beneficial. In this therapy, you can acquire valuable skills for managing profound and long-enduring stress, ultimately breaking free from the cycle.
Good to Know!
The likelihood of experiencing an immune system crash and developing silent inflammation is elevated in individuals with stressful experiences during childhood or adolescence. A disrupted stress processing system can be a long-term consequence, but it is a condition that can also be facilitated through psychosomatic psychotherapy [2].
In a Nutshell
PNI explores how stress impacts the immune system; research shows it is significant. Prolonged psychological stress raises inflammation markers, increasing the risk of long-term illnesses. This weakens our immune system and makes us more vulnerable to infections.
This, in turn, affects mental well-being, creating a vicious cycle. This can relate to endometriosis. However, regular relaxation techniques and focused psychotherapy can offer a way out and long-term relief.
References
- Schmoll et al. 1996 “Psychoneuroimmunology.” Compendium of Internal Oncology.
- Planet Knowledge. 2020. “Psychoneuroimmunology: How emotions influence the immune system.“ https://www.planet-wissen.de/gesellschaft/medizin/psychosomatik/psychoneuroimmunologie-100.html (Zugriff 18.04.2022)
- Schubert, C. 2013. “Psychoneuroimmunology and susceptibility to infection.” Journal of Complementary Medicine 5: 17-23
- Nadja Tariverdian. 2011. peripheral immune status, psychosocial stress and neuroendocrine-immunological circuits in endometriosis. Dissertation submitted to the Faculty of Medicine Charité – Universitätsmedizin Berlin.
- Shigesi, N. et al. 2019. „The association between endometriosis and autoimmune diseases: a systematic review and meta-analysis.“ Human Reproduction Update 25 (4): 486-503.
Have you experienced the impact of stress on your immune system?
Share your experience with us in the comments below.
- Endometriosis and Nickel Allergy: Are There Connections? - 5. October 2023
- Psychoneuroimmunology – Immune System in Permanent Stress - 10. September 2023
- Unlocking the Mystery of Vulvodynia: Understanding Pubic Pain - 9. September 2023