Polycystic Ovary Syndrome (PCOS): Definition, Symptoms, Diagnosis, Therapy, and Relationship to Endometriosis
PCOS, which stands for ‘Polycystic Ovary Syndrome’ is the prevalent endocrinological disorder among individuals with reproductive cycles. It is a multisystem condition primarily impacting the ovaries and endometrium, while also influencing insulin balance.
Furthermore, PCOS results in diminished fertility and an elevated risk of pregnancy complications. Despite sharing numerous symptoms with endometriosis, PCOS is a distinct disorder in its own regard.
Background: What is PCOS?
Polycystic ovary syndrome affects approximately 5 to 15% of individuals with reproductive cycles, varying by source. The onset of this condition often occurs during adolescence, shortly after the first menarche. However, diagnosis frequently requires several years.
Despite being a gynecological disorder, PCOS exhibits a wide array of symptoms, contributing to its classification as a multisystemic condition. Beyond impacting the menstrual cycle and fertility, these symptoms can also lead to manifestations like type II diabetes. Alongside its adverse effects on fertility, PCOS frequently results in a substantial reduction in quality of life [1].
This article aims to provide insights into the following aspects of PCOS:
- Symptoms and causes of PCOS.
- Diagnosis and treatment options for PCOS.
- Differentiating PCOS from other related diseases.
- The impact of PCOS on fertility and the desire to have children.
Symptoms: How Does PCOS Manifest Itself?
PCOS symptoms encompass a range of both specific and non-specific indications, typically emerging during puberty and progressing over time.
- No or Irregular Menstrual Bleeding: Women with PCOS often experience cycles without ovulation, leading to a complete absence of menstrual bleeding or only light spotting.
- Reduced Fertility: Ovulation irregularities contribute to reduced fertility in those with PCOS.
- Masculinization: Some individuals may develop increased facial, chest, and abdominal hair growth, alongside male-pattern hair loss on the scalp. A deeper voice and augmented muscle mass can also manifest. Additionally, small breast size is common.
- Acne: Severe acne, persisting into adulthood, is a prevalent symptom among those affected.
- Overweight: A significant number of PCOS patients struggle with excess weight, which is further complicated by hormonal imbalances that impede weight loss.
- Skin Symptoms: Darkened skin around the armpits and neck, sometimes exhibiting a leathery appearance, is observed, particularly in individuals with darker skin tones.
- Sleep Apnea: Breathing difficulties during sleep, leading to pauses in breathing, can result from PCOS.
- Depression, Anxiety, and Eating Disorders: PCOS patients have a higher incidence of these conditions compared to healthy women of similar age groups, affecting 24 to 48 percent of individuals.
Untreated, PCOS can give rise to other urgent medical concerns:
- Diabetes Mellitus Type 2: Between 50 to 75% of PCOS patients exhibit precursors to Type 2 Diabetes Mellitus.
- Endometrial Carcinoma: Thickening of the endometrium elevates the risk of endometrial carcinoma formation in numerous affected women.
- Cardiovascular Disease: Increased fat accumulation around the trunk and altered cholesterol levels amplify the risk of cardiovascular disease.
- Non-Alcoholic Fatty Liver: PCOS women are at a significantly heightened risk of non-alcoholic fatty liver, independent of their body weight.
Causes: What Leads to Polycystic Ovary Syndrome?
Despite its widespread prevalence, the exact cause of PCOS remains elusive. Studies propose that an enzymatic malfunction involved in male hormone production may underlie PCOS, leading to elevated male hormone concentrations and consequently contributing to several symptoms outlined earlier.
Moreover, some male hormones are converted into estrogen, causing an overall estrogen level increase due to inadequate progesterone production that could otherwise balance these elevated estrogen levels. This process contributes to symptoms like uterine lining thickening.
As of current understanding, factors triggering PCOS encompass:
Genetic Factors
Environmental Influences
Obesity
Diagnosis: How is PCOS Identified? (Distinguishing from Other Conditions)
Diagnosing PCOS can be challenging due to the range of symptoms, which can differ in intensity among individuals. Moreover, despite its prevalence, PCOS is often overlooked as a potential cause of symptoms. Key diagnostic measures to investigate suspected PCOS include:
- Medical Examination
- Hormone Level Assessments (Blood Tests)
- Ultrasound Examination
According to the Rotterdam criteria, PCOS is diagnosed when at least two of the following three criteria are met:
- Oligo- or Anovulation: Absence of irregularity of ovulation, determined through progesterone level assessment.
- Hyperandrogenism: Elevated androgen levels confirmed through physical examination or blood tests.
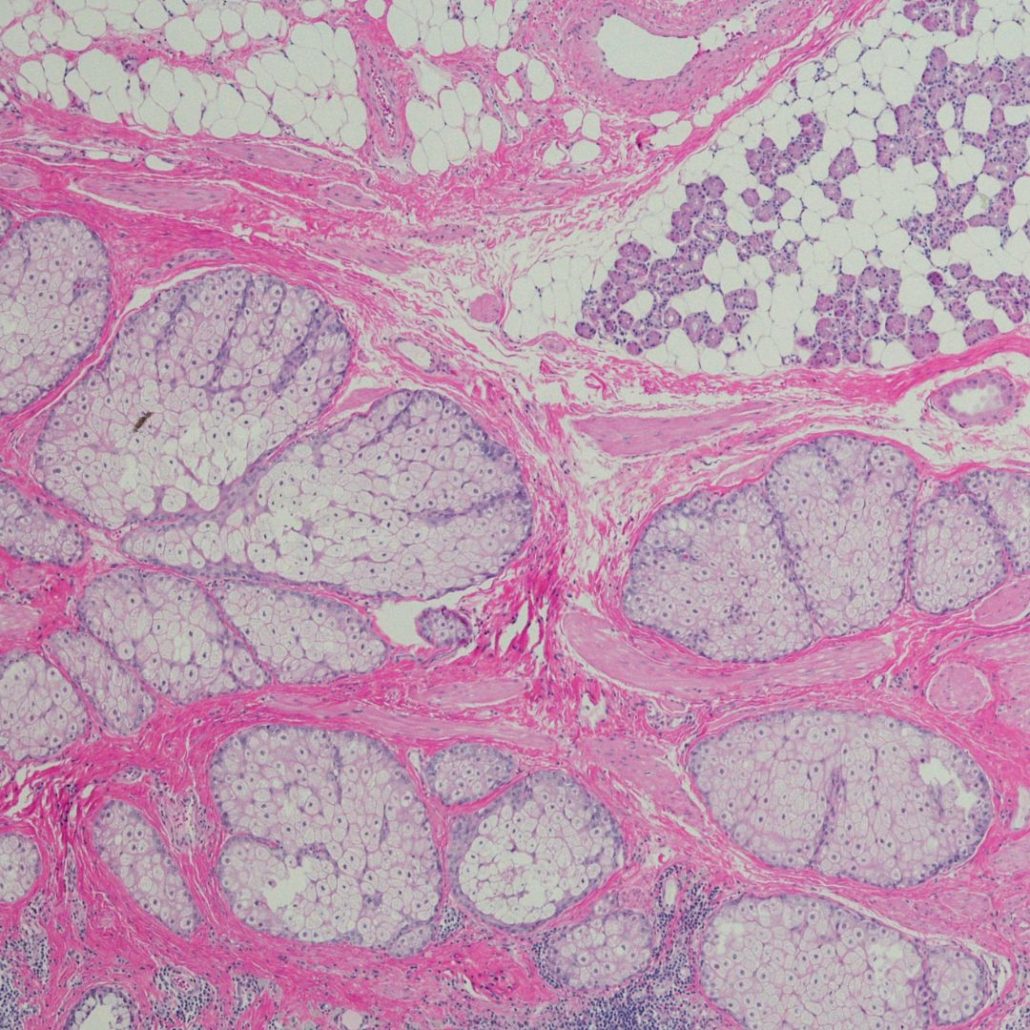
- Polycystic Ovaries (PCO) – also called polyfollicular ovaries: Ultrasound imaging to identify cysts in the ovarian region resulting from disrupted follicle maturation.
Additionally, other potential causes must be ruled out, including [4]:
- Congenital adrenal hyperplasia
- Androgen-producing tumors
- Cushing’s syndrome
Precise differentiation is crucial as there are other forms of follicle maturation disorders, which can be overwhelming for individuals, particularly those dealing with infertility.
If patients fulfill the above criteria, further assessments are recommended for clarification:
- Blood pressure measurement: PCOS is linked to increased cardiovascular disease risk, including hypertension.
- Blood tests (fasting): Triglycerides, HDL and LDL cholesterol, and possibly liver enzyme levels.
- Thyroid function evaluation: TSH, TPO-AK tests identify autoimmune thyroid disorders.
- Insulin resistance: assessment through fasting blood sugar and insulin levels.
- BMI determination: in cases of significant overweight, assessment for sleep disorders including sleep apnea (breathing pauses during sleep).
Therapy: How Can PCOS Be Managed?
Similar to endometriosis, PCOS lacks a causal treatment. Concrete therapeutic approaches depend on several factors:
- Symptom Manifestation: Which symptoms are present and how severe are they? How much do they affect the patient?
- Patient’s Age
- Phase of Life: Is family planning completed? Is pregnancy being sought now or in the future?
For frequently encountered PCOS symptoms, the following therapeutic strategies are considered:
General Symptom Reduction Measures
- Hormonal Treatment: Birth control pills, especially those with progesterone or combined estrogen-progesterone formulations, are used to balance hormone levels and alleviate excess male hormones. This can decrease the risk of endometrial cancer, normalize the menstrual cycle, and reduce body hair and acne. However, this approach is NOT suitable for women trying to conceive.
- Metformin: Used for type II diabetes, it enhances insulin sensitivity. It aids in weight reduction and cycle normalization, particularly beneficial for infertility cases.
- Surgery: Ovarian wedge resection destroys areas producing male hormones. This can enhance pregnancy likelihood.
Obesity Treatment:
Given elevated insulin levels in PCOS, the following measures help:
- Regular Exercise: Aim for 30 minutes of moderate activity (walking, cycling) on 5 days, with more intense exercises (jogging, swimming) twice weekly.
- Dietary Changes: Reduce carbohydrates; focus on whole grains, fruits, and vegetables.
Please note: These measures primarily benefit overweight women by targeting insulin levels. Nevertheless, exercise promotes overall physical and emotional well-being.
Excessive Body Hair Treatment:
Apart from medical treatments, increased body hair can be managed with:
- Depilatory Creams
- Laser Hair Removal
- Intense Pulsed Light (IPL)
- Waxing and Sugaring
PCOS and Endometriosis: Understanding the Connection
Endometriosis, akin to PCOS, falls within gynecological disorders but exhibits multisystemic impacts [5]. Prominent endometriosis symptoms encompass:
- Menstrual irregularities, often involving excessive bleeding.
- Initially menstruation-linked pain that can evolve into chronic discomfort.
- Diminished fertility.
- Pain beyond the abdomen due to endometriosis lesions spreading beyond the pelvic region.
- Elevated risk of depression.
PCOS and endometriosis do share certain similarities, yet they are distinct conditions. Nonetheless, some individuals may experience both simultaneously. In such cases, treatment coordination becomes crucial to effectively alleviate symptoms of both disorders.
Summary:
PCOS, or polycystic ovary syndrome, belongs to gynecological disorders. Despite affecting potentially up to 20 percent of women of reproductive age based on different assessments, PCOS remains relatively unfamiliar.
Untreated PCOS can result in substantially impaired fertility and complications during pregnancy. Fortunately, effective treatment options exist for managing most symptoms, offering PCOS patients a positive outlook for achieving a healthy pregnancy.
While PCOS and endometriosis present comparable symptoms, they are distinct conditions. Yet, there are instances where individuals are simultaneously impacted by both ailments.
References
- FHA, Frauenheilkunde aktuell, 4/2018; Ein PCOS geht alle an
- https://www.msdmanuals.com/de-de/heim/gesundheitsprobleme-von-frauen/menstruationsst%C3%B6rungen-und-abnormale-scheidenblutungen/polyzystisches-ovarialsyndrom-pcos
- GynDepesche 1/2008; The fight against PCOS and its consequences
- Medical Tribune: https://www.medical-tribune.de/medizin-und-forschung/krankheitsbild/gynaekologie/polyzystisches-ovarsyndrom
- Gynecology and Obstetrics, Springer Verlag, 2006.
Andreas D. Ebert; Endometriosis, A Guide for the Practice; De Gruyter
Do you suspect that you might have PCOS, or have you already received a diagnosis?
Share your experience with us in the comments section.
- Endometriosis and Migraine: What is the Connection Between the Two Conditions? - 8. October 2023
- Endometriosis and Migraine: What is the Connection Between the Two Conditions? - 8. October 2023
- Can I Inherit Endometriosis? - 7. October 2023