Endometriosis at the Colon Rectum
Endometriosis affecting the colon is the most prevalent form of bowel-related endometriosis. In cases of rectovaginal endometriosis, where the lesions settle between the colon and the vagina, the rectum is commonly involved as well. Interestingly, the level of endometriosis does not always correlate directly with the intensity of pain or discomfort experienced, meaning even small lesions can lead to severe pain, while large lesions may not necessarily cause more intense discomfort. However, research indicates that pain is usually triggered when endometriosis penetrates the tissue by more than 5 mm, and particularly severe pain arises when the depth of infiltration exceeds 10 mm [1]. This condition is referred to as deep infiltrating endometriosis.
Among the affected regions, the rectum and the transition area between the sigmoid colon and the rectum are most frequently impacted. Comparatively, occurrences of endometriosis in the appendix or small intestine are less common [2]. Consequently, experiencing bowel problems due to endometriosis, including bowel pain, is a valid concern, as we will further explore.
Symptoms of Endometriosis of the Rectum
One characteristic sign of endometriosis at the rectum is bleeding from the bowel, which coincides with the patient’s menstrual cycle [4]. However, the specific symptom is only observed in approximately 30% of cases [3].
Diagnosing endometriosis can sometimes be challenging due to symptoms resembling those of other gastrointestinal disorders. Nevertheless, there are several common complaints reported by patients [4]:
- Chronic constipation, resulting from the narrowing of the rectum due to endometriosis.
- Experiencing small and solid bowel movements, often likened to “rabbit stool”.
- Heightened constipation during the menstrual period, caused by additional swelling of the rectum
- A few days after the period, the stool may become more liquid and patients may briefly experience relief from constipation
Numerous symptoms associated with colon or rectal infestations can also manifest independently. These symptoms may include:
- Pain during sexual intercourse (dyspareunia), resulting in a significant loss of libido due to severe discomfort experienced.
- Development of an “endobelly”, characterized by a severely distended abdomen, leading to intense pain.
- Nausea.
- Pain, especially in the lower back.
- Bowel evacuation disorders such as diarrhea.
Additionally, if endometriosis affects the appendix, it can give rise to symptoms similar to those of appendicitis.
Diagnosis
Diagnosing intestinal endometriosis presents a considerable challenge due to the array of symptoms that can overlap with those of other diseases. The initial step involves careful observation, and the patient is often asked to assess their pain on a pain scale. However, based solely on this, only a preliminary diagnosis can be established.
Similar to rectovaginal endometriosis, rectovaginal palpation plays a crucial role in the diagnostic process. During the examination, the doctor simultaneously palpates the vagina and rectum using one finger each. This approach helps to assess the extent to which endometriosis lesions have affected the rectum. Given that the rectum is the most common site of endometriosis, this examination holds significant importance. It is important to note that endometriosis lesions in other parts of the colon cannot be detected through this method, but they are much less frequent occurrences.
To gather more information, endosonography of the rectum can be performed. Additionally, MRI can be utilized to assess the extent of the adhesions, and determine whether the endometriosis foci have penetrated the bowel wall, potentially necessitating bowel resection [3].
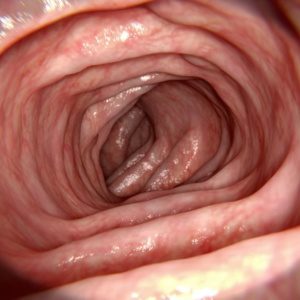
A colonoscopy is also a standard procedure in the diagnosis of intestinal endometriosis. It can detect endometriosis affecting the inside of the bowel, but it may not identify endometriosis located on the outside of the bowel. Consequently, if a colonoscopy appears normal, it does not automatically rule out the possibility of bowel involvement.
However, the most reliable and accurate method for diagnosing intestinal endometriosis is through laparoscopy [3]. This surgical procedure allows for precise localization of endometriosis on the colon and rectum and provides a clear assessment of the extent of the affected area. Importantly, certain foci of endometriosis might not be visible on ultrasound or endosonography, making laparoscopy indispensable for a comprehensive evaluation [3]. This surgical procedure allows for precise localization of endometriosis on the colon and rectum and provides a clear assessment of the extent of the affected area.
Given the significance of the diagnosis and potential treatment options, patients are informed in advance about all the possible procedures related to rectal endometriosis. For instance, in cases where bowel resection is necessary, there is a chance that the patient might wake up with a stoma, which would need to be worn for several weeks until the bowel is repositioned.
Treatment
In the treatment and management of endometriosis affecting the colon and rectum, various factors must be considered, including the patient’s age, desire to have children, the extent of endometriosis, the involvement of other organs, and the presence of symptoms such as pain [5].
According to the guidelines, surgical treatment may not be necessary if endometriosis of the bowel is an incidental finding and there are no symptoms. However, this type of endometriosis often presents with significant pain and gastrointestinal issues. Therefore, seeking treatment at an endometriosis center, which collaborates closely with other specialists like colon surgeons and urologists, is recommended. Pain relief medications can be prescribed, and hormonal therapies, such as progestins, combined pills, GnRH agonists/antagonists, or levonorgestrel-releasing IUDs [5] may be beneficial in alleviating symptoms, However, where endometriosis involves the bowel, surgery is often the preferred and most effective long-term treatment to improve pain and fertility [6]. Deciding on the best course of action is a personalized decision that should be made in consultation with the endometriosis center, considering the individual’s circumstances and preferences.
After Laparoscopy
If endometriosis lesions on the bowel wall can be removed without breaching the bowel, patients do not need to worry about a partial resection of the bowel. However, if a segment of the bowel had to be removed during the surgery, the patient might have to live with a stoma, an artificial bowel outlet, for a few weeks or months to facilitate better healing of the operated areas. Subsequently, the bowel can be repositioned. It is challenging to predict with certainty which option will be required before the operation, leading to discussions about the possibility of a stoma.
Although the prospect of an artificial bowel outlet might be worrisome for many patients, a study indicates that 44.6% of women with a desire to have children after a bowel resection were able to conceive without any complications. The removal of the affected bowel section, therefore, enhances fertility in numerous patients. Furthermore, noticeable improvements in symptoms lead to a significant enhancement in the quality of life for those individuals [1]. Post-surgery, ongoing treatment options are discussed with the treating physicians. For many patients, drug therapy, such as using progestogens, may be considered. Additionally, patients can positively influence their well-being through dietary adjustments and engaging in activities such as yoga.
Are you interested in the topic of endometriosis of the bowel and would like to access further information about it? Then feel free to download our Endo-App and receive helpful tips from our experts.
References
- Johann, Silke; Eberhard, Markus: Surgery for endometriosis-associated pain and deep infiltrating endometriosis. Clinical images, surgical planning, techniques. (=Gynecology 3/2012), PDF: https://www.rosenfluh.ch/gynaekologie-2012-03/chirurgie-bei-endometrioseassoziierten-schmerzen-und-tief-infiltrierender-endometrie.
- Ruffo G, Rossini R. The outcomes of laparoscopic resection of bowel endometriosis. Curr Opin Obstet Gynecol. 2013 Aug;25(4):302-7. doi: 10.1097/GCO.0b013e3283630e26. PMID: 23817230.
- Keckstein, J. Endometriosis in the intestinal tract. coloproctology 39, 121–133 (2017). https://doi.org/10.1007/s00053-017-0144-5.
- Possover, Marc Prof. Dr. med.: Endometriosis – clinic and therapy. Date retrieved: 14. Mai 2021, von (PDF): https://www.hirslanden.ch/content/dam/klinik-hirslanden/downloads/de/centers/zentrum-für-neuropelveologie/neuropalveologie-endometriose-klinik-und-therapie-de.pdf
- Tiringer, D, Husslein, H, Küssel, L, Wenzl, R. Diagnosis and therapy of “rectovaginal” or deep infiltrating “intestinal endometriosis”. 37th ed. 1/2019. Available from: https://www.kup.at/kup/pdf/14384.pdf
- Mangler, M., Loddenkemper, C., Lanowska, M., Bartley, J., Schneider, A., Köhler, C. A combined surgical approach to rectovaginal endometriosis therapy based on histologic findings. Journal of Gynecological Endocrinology2008; 2 (2) (Ausgabe für Österreich). Gablitz. Available from: https://www.kup.at/kup/pdf/7119.pdf
- “Take yourself and your endometriosis seriously. You are not imagining things!” - 7. November 2023
- Interview with Endometriosis Patient Nina - 7. November 2023
- Interview with Endometriosis Patient Nina - 7. November 2023