Cysts: Understanding the Different Types
The term cyst is derived from the Greek word for “bladder” (kystis). When a cyst forms in your body, it creates a cavity within the tissue, also known as a capsule by physicians. The appearance of the capsule can vary greatly, with cysts ranging from just a few millimeters to several centimeters in size – some even containing multiple chambers [1]. Today, I’ll discuss the different types of cysts that can occur in women and why one specific type – the chocolate cyst – is significant in endometriosis.
5 Types of Cysts Explained
Cysts manifest in various ways and can be influenced by multiple factors. Some are congenital, while others develop due to hormonal influences or as a result of certain medical conditions. Physicians use different terms to distinguish between cyst types, which is crucial for prompt and accurate diagnosis, as well as for initiating suitable treatment. Let’s take a closer look at these five types of cysts.
1. Congenital Cysts
Some cysts are present from birth and are known as congenital cysts. Among them are dermoid cysts, also referred to as teratomas. These cysts originate from germ cells, classifying them as germ cell tumors. What makes dermoid cysts intriguing is their potential to contain bone, hair, and even teeth [2]. This has led to the misconception of calling them the “lost twin,” but in reality, they are not undeveloped offspring but a result of the maldevelopment of their own embryonic tissue. Dermoid cysts consist of primitive cells from the embryo, serving as the foundation for various tissue and cell forms. Laparoscopy is the common method for removing dermoid cysts. Please note: It is worth noting that this form of cysts can also appear later in life, making them not exclusively congenital. An acquired dermoid cyst develops from a benign tumor that is equipped with skin cells and sebaceous glands. When sebum formed inside the cyst cannot drain away, a cyst may form [3].
Good to know!
Germ cell tumors are more commonly found in younger women [2]. However, it is important not to be alarmed by the term “tumor” as most dermoid cysts are benign in nature.
2. Functional Cysts
Among the various types of cysts, functional cysts are the most commonly observed changes in the ovaries. These cysts are formed from structures with cavities that serve a normal purpose in the body and are significantly influenced by hormones. Consequently, during periods of major hormonal fluctuations, such as puberty and menopause, the risk of developing functional cysts increases [4].
The following types of functional cysts are frequently encountered:
- Follicular cyst: Also known as a vesicular cyst, this type forms when the follicle, the shell in which the eggs mature, fills with fluid and transforms into a cyst. This can occur if ovulation does not take place [4]. Follicular cysts can remain unnoticed for a while, often regress on their own, and occasionally cause lower abdominal pain.
- Corpus luteum cyst: Commonly known by this name, the corpus luteum cyst forms when blood enters the corpus luteum. The corpus luteum is the remaining shell of the egg after ovulation and prepares the body for a potential pregnancy by producing sex hormones, estrogen, and progesterone [4]. Symptoms of a corpus luteum may include abdominal pain or a missed menstrual period.
- Lutein cyst: This type of cyst can occur on both ovaries simultaneously and causes significant menstrual symptoms and intermenstrual bleeding. Lutein cysts are often associated with hormone therapy used for fertility treatments [5].
Influence of Hormones on Functional Cysts?
Hormones play a pivotal role in your body, ensuring the regularity of your menstrual cycle and fertility. However, certain circumstances can lead to undesirable developments, including the promotion and maintenance of functional cysts. The hormones involved in this process are primarily estrogen and progestins, also known as corpus luteum hormones, which are ovarian hormones produced by the ovaries [6]. Additionally, gonadotropins like follicle-stimulating hormone (FSH) and luteinizing hormone (LH), play significant roles. FSH stimulates follicle maturation and estrogen production within the follicle, while LH triggers ovulation [7].
Risk Factors for Functional Cysts
Interfering with your hormonal balance can increase the risk of developing functional cysts [5].
Some of the risk factors include:
- Infertility treatment: Therapies aimed at increasing the production of HCG (human chorionic gonadotropin) during fertility treatments may promote cyst formation in the female reproductive system [5].
- Pregnancy: During pregnancy, the corpus luteum significantly increases its production of hormones to support your pregnancy, increasing the likelihood of cysts.
- Hypothyroidism: Did you know that hypothyroidism stimulates the release of a hormone that is meant to stimulate the thyroid gland? However, this hormone is similar to the one that stimulates egg production in your ovaries, potentially promoting cyst development.
Do Functional Cysts Require Surgery?
 Functional cysts can be quite common even in women with regular menstrual cycles. Gynecologists often detect them during physical examinations, for example during a vaginal ultrasound [8]. In most cases, these cysts resolve on their own over weeks or months. However, if they persist and cause intense symptoms, regular monitoring by a gynecologist is advised. While taking birth control pills does not typically cause cyst regression [9], your doctor may recommend surgical removal of the cyst if necessary
Functional cysts can be quite common even in women with regular menstrual cycles. Gynecologists often detect them during physical examinations, for example during a vaginal ultrasound [8]. In most cases, these cysts resolve on their own over weeks or months. However, if they persist and cause intense symptoms, regular monitoring by a gynecologist is advised. While taking birth control pills does not typically cause cyst regression [9], your doctor may recommend surgical removal of the cyst if necessary
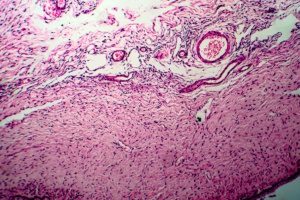
3. Bleeding Cysts
Cysts typically contain fluid within their cavity, which can be tissue fluid, pus, or sebum. However, some cysts can also contain blood, earning them the name “bled-in-cysts”. Essentially, any functional cyst has the potential to bleed in. A clear example of this is the corpus luteum cyst. In this case, the cyst develops when the follicle bleeds following ovulation, and the accumulated blood forms a cavity.
Another scenario for the formation of bleeding cysts is when an increase in fluid volume damages a blood vessel in the cyst wall, causing blood to enter the cyst.
It is important to distinguish these types of cysts from endometriosis cysts.
4. Chocolate Cysts
If you have been diagnosed with endometriosis, you may have encountered the term “chocolate cyst”. This phenomenon belongs to the category of functional cysts. Also known as endometriosis cysts or endometriomas, they are exclusive to endometriosis cases. These cysts contain old and thickened blood that accumulates due to bleeding or during menstruation. Their contents give them a brownish appearance, earning them the name “chocolate cysts.” The exact process of how chocolate cysts develop is still not fully understood. Studies indicate that endometriomas can be detected in up to 44% of endometriosis patients and are often associated with deep infiltrating endometriosis [10]. If you have been diagnosed with a chocolate cyst through ultrasound or palpation, several treatment options are available, depending on the initial findings. Surgical removal of the cyst is a common approach, which can alleviate pain and potentially increase the likelihood of pregnancy [11, 12].
Good to know!
In addition to surgical removal of the chocolate cyst, hormonal treatment is also considered an option. However, it is important to note that it does not completely dissolve the cyst but may lead to a reduction in size at best [13]. Would you like to learn more about chocolate cysts? Then read our blog post titled: “Endometriosis Cyst: the Chocolate Cyst.”
5. Indeterminate Cysts
In some cases, cysts cannot be clearly identified and classified into a specific group. When the cause is uncertain or there is a suspicion of a possible carcinoma, which refers to a malignant transformation, the cyst is typically removed through a surgical procedure. Various symptoms and ultrasound examination may provide indications of a potentially malignant finding. The definitive diagnosis is made by the physician after tissue samples have been obtained during the operation and subsequently examined in a laboratory. Don’t worry: It is important to note that a malignant cyst finding is very rare, especially at a young age. So you don’t need to immediately fear cancer in relation to the cysts mentioned above.
Polycystic Ovary Syndrome (PCOS)
Polycystic ovary syndrome is the most common hormonal disorder in women of childbearing age. Unlike the types of cysts mentioned earlier, PCOS is characterized by the presence of many small cysts forming in the ovaries. Physicians refer to this condition as polycystic ovaries (PCO) [14]. In addition to visibly enlarged ovaries, individuals with PCOS may experience menstrual irregularities or have elevated levels of male hormones (hyperandrogenism). The hormonal disorder also differs from the classic types of cysts in terms of treatment. To regulate the menstrual cycle, doctors recommend weight reduction and regular exercise. Antiandrogenic therapy, drugs that promote follicle maturation, and the antidiabetic drug metformin have shown promise as well [15]. According to one study, the use of combined contraceptives may also be beneficial. In this study, 36 patients with PCOS significantly reduced their follicle count (by 40.3%) with 20 μg ethinylestradiol /3 mg drospirenone for at least one year [16].
Important Note: If you have been diagnosed with endometriosis and/or a cyst, it is essential to discuss hormonal therapy with your gynecologist.
In a Nutshell
Cysts are cavities enclosed by a capsule and containing fluids or soft material. Cysts can potentially develop anywhere in the body. Among women, ovaries are the common site. Individuals with endometriosis typically encounter functional cysts, influenced by hormones yet often not requiring treatment. Notably, the term “chocolate cysts” refers to such functional cysts filled with menstrual blood. While typical functional cysts recede within weeks or months, chocolate cysts persist and necessitate surgical removal. Treatment determination, dependent on cyst type and symptoms, is made by your physician.
Have you downloaded the Endo-App? It provides comprehensive information on endometriosis.
Good to know!
Endometriosis cysts may indicate either peritoneal endometriosis or deep infiltrating endometriosis [17]. Therefore, it is crucial for your doctor to conduct thorough examinations (e.g., palpation or ultrasound examination).
References
- Zyste | Gesundheitsinformation.de
- Diedrich, Klaus. Gynecology and obstetrics (Springer textbook) (German Edition) (p.246). Springer Berlin Heidelberg. Kindle version.
- Eierstockzysten (Ovarialzysten) – gesund.bund.de
- Eierstockzysten (Ovarialzysten) | Gesundheitsinformation.de
- Eierstockzyste » Was sind die häufigsten Ovarialzysten? » (frauenaerzte-im-netz.de)
- Diedrich, Klaus. Gynecology and obstetrics (Springer textbook) (German Edition) (p.245). Springer Berlin Heidelberg. Kindle version.
- Gonadotropine (LH) | Gesundheitsportal
- American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology. Practice Bulletin No. 174: Evaluation and Management of Adnexal Masses. Obstet Gynecol. 2016 Nov;128(5):e210-e226. doi: 10.1097/AOG.0000000000001768. PMID: 27776072.
- Grimes DA, Jones LB, Lopez LM, Schulz KF. Oral contraceptives for functional ovarian cysts. Cochrane Database Syst Rev. 2014 Apr 29;(4):CD006134. doi: 10.1002/14651858.CD006134.pub5. PMID: 24782304.
- Cranney R, Condous G, Reid S. An update on the diagnosis, surgical management, and fertility outcomes for women with endometrioma. Acta Obstet Gynecol Scand. 2017 Jun;96(6):633-643. doi: 10.1111/aogs.13114. Epub 2017 Mar 11. PMID: 28186620.
- Pais AS, Flagothier C, Tebache L, Almeida Santos T, Nisolle M. Impact of Surgical Management of Endometrioma on AMH Levels and Pregnancy Rates: A Review of Recent Literature. J Clin Med. 2021 Jan 22;10(3):414. doi: 10.3390/jcm10030414. PMID: 33499120; PMCID: PMC7865255.
- Angioni, S., Scicchitano, F., Sigilli, M., Succu, A. G., Saponara, S., & D’Alterio, M. N. (2021). Impact of Endometrioma Surgery on Ovarian Reserve. In Endometriosis Pathogenesis, Clinical Impact and Management (pp. 73-81). Springer, Cham.
- Endometriosezyste – die Schokoladenzyste – Endometriose
- Polyzystisches Ovar Syndrom | Gesundheitsportal
- Diedrich, Klaus. Gynecology and obstetrics (Springer textbook) (German Edition) (p.108). Springer Berlin Heidelberg. Kindle version.
- Park CH, Chun S. Influence of combined oral contraceptives on polycystic ovarian morphology-related parameters in Korean women with polycystic ovary syndrome. Obstet Gynecol Sci. 2020 Jan;63(1):80-86. doi: 10.5468/ogs.2020.63.1.80. Epub 2019 Dec 20. PMID: 31970131; PMCID: PMC6962579.
- Exacoustos C, Zupi E. A new era in diagnosing adenomyosis is coming. Fertil Steril. 2018 Oct;110(5):858. doi: 10.1016/j.fertnstert.2018.07.005. PMID: 30316431.
- Pharmaceutical Companies and Their Influence on Scientific Research - 7. October 2023
- Identification of a Genetic Factor Linked to Endometriosis Development and Potential Therapeutic Targets - 6. October 2023
- Identification of a Genetic Factor Linked to Endometriosis Development and Potential Therapeutic Targets - 6. October 2023
