Endometriosis Affecting the Pelvic Walls
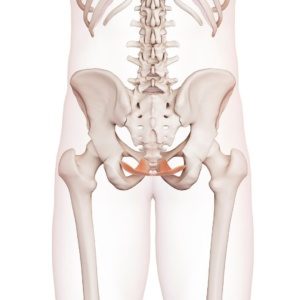
Endometriosis is a prevalent common gynecological ailment, ranking second only to fibroids in statistical prevalence [1]. Its hallmark symptoms, including abdominal discomfort, infertility, and painful menstruation, emerge due to the growth of tissue akin to endometrium outside the uterus. This expansion can extend to impact the pelvic walls.
Today, I will delve into the symptoms arising from endometriosis affecting the pelvic walls, along with medical interventions employed by doctors to address this condition.
Brief Exploration: Endometriosis Across Pelvic and Non-Pelvic Domains
Within the realm of endometriosis, experts delineate various forms, a classification that profoundly informs treatment strategies and ongoing care.
The ensuing variants of endometriosis can manifest:
- Endometriosis Genitalis Interna: This variant entails lesions embedded within the myometrium – essentially, within the uterine wall’s muscular layer. Medically, this occurrence is referred to as “adenomyosis uteri” [1].
- Endometriosis Genitalis Externa: This is the most prevalent form, where foci also lie within the pelvic realm, albeit outside the uterus. Lesions might emerge on the ovaries or within the “Douglas space”, an indentation situated between the rectum and uterus [1].
- Endometriosis Extragenitalis: This presentation extends beyond the pelvic precinct. Consequently, endometriosis lesions can surface in various non-pelvic regions, affecting the intestine, bladder, and ureters, and even extending to the brain.
Good to know!
Endometriosis can manifest both within and beyond the pelvic region, The pelvic cavity, encompassing the rectum, urinary bladder, vagina, uterus, and ovaries, is a commonly afflicted site for endometriosis lesions.
Endometriosis on the Pelvic Walls: Symptoms
Endometriosis can give rise to a diverse array of symptoms. Much like other conditions, there exist key symptoms that unmistakably point to endometriosis. Simultaneously, there are also less specific symptoms that could be linked to endometriosis, yet they are equally plausible outcomes of other factors.
Distinctive endometriosis symptoms:
- Painful menstrual bleeding (dysmenorrhea) [2]
- Painful urination (dysuria) [2]
- Defecation difficulties (dyschezia) [2]
- Pain during sexual intercourse (dyspareunia) [2]
- Infertility (sterility) [2]
Less specific endometriosis symptoms:
Indications of Pelvic Wall Endometriosis

Beyond the previously mentioned, specific and non-specific symptoms, there are distinct signs that may point to adhesions on the pelvic walls. For instance, individuals grappling with retroperitoneal endometriosis – where structures behind the peritoneum are affected – commonly report back pain, particularly during menstruation. This discomfort may stem from endometriosis tissue infiltrating the pelvic wall or coccyx.
A phenomenon that can accompany pelvic wall endometriosis is leg pain. The lateral spread of lesions towards the pelvic wall contributes to this occurrence.
The sacral plexus, a nerve plexus, might be impacted in such scenarios. This could lead to leg pain, alongside potential neurological manifestations like reduced sensation or limited mobility.
In certain cases, patients voice discomfort in the buttocks or experience sciatica – an affliction emanating from the sciatic nerve [4].
Good to know!
Additional symptoms often manifest when pelvic wall endometriosis encroaches upon other anatomical structures, like the ureter. Such occurrences arise when adhesions on the pelvic wall “constrict” the ureter. This constriction might lead to urinary retention, evident through back pain, potentially showcasing kidney obstruction in ultrasound examinations. Furthermore, endometriosis nodules and adhesions can form amid the pelvic wall and intestines, potentially impeding normal bowel function.
Discomfort during sexual intercourse can also trace its origins to pelvic wall endometriosis. This might stem from two sources: the movement of inflamed endometriosis tissue during deep penetration and the potential development of pelvic floor tension due to severe pain.
Pelvic Wall Endometriosis: Diagnostic Insights
A vital advisory prevails: In the presence of persistent discomfort, especially during menstruation, or if you have a pre-existing endometriosis diagnosis but encounter escalating or novel symptoms, seeking medical consultation is imperative, Though a comprehensive diagnostic process, your physician can discern the localization and severity of your endometriosis.
The diagnostic journey comprises several pivotal steps:
- Anamnesis: Initially, the doctor inquires about your symptoms and overall health. Your family history might also be explored, as genetic factors seem to play a significant role. Notably, specific genes have been identified in studies that foster endometriosis development [5].
- Examination: Skillfully palpating the pelvic walls via simultaneous rectal and vaginal palpation, the physician can detect foci. Unfortunately, finding foci might also trigger discomfort. An ultrasound is commonly conducted as well, although, it is essential to recognize that this is not foolproof. Not all endometriosis foci are palpable or visible through ultrasound.
- Imaging: Diverse diagnostic techniques are employed to unearth endometriosis. The chosen approach hinges on the suspected form and severity. Ultrasound can visualize adhesions, while magnetic resonance imaging (MRI) [6] has garnered attention due to its radiation-free capability to yield precise images of endometriosis lesions, aiding surgical planning [7].
- Laparoscopy: This quintessential procedure is adept at reliable endometriosis diagnosis. Under general anesthesia, a camera is introduced into the abdomen via a small tube. The number and extent of adhesions are evaluated [8].
Please note: spotting endometriosis lesions within the pelvic wall is not always straightforward, underscoring the significance of a skilled surgeon. Post-focus removal, laboratory analysis verifies the presence of endometrial tissue. - Severity Classification: Categorization into a severity tier determines subsequent steps. Different classifications are used, with pelvic wall endometriosis typically evaluated using the ENZIAN classification. This aids in identifying deep infiltrating endometriosis, with nodes sized and compartment B pinpointing pelvic wall involvement [2].
What are the Treatment Approaches for Pelvic Wall Endometriosis?
In the presence of pelvic wall endometriosis, your medical provider will instigate an appropriate course of treatment. The chosen approach hinges on the extent of adhesions. If your quality of life is hampered by discomfort – for instance, enduring abdominal and back pain during every menstrual cycle – surgery might be the optimal path. Surgical intervention is also recommended if adjacent organs are impacted, as evidenced by symptoms like painful urination or urinary retention, Given the proximity of sensitive structures, the surgeon’s expertise is pivotal in ensuring precise tissue removal.
Nonetheless, the treatment of pelvic wall endometriosis must be approached on a case-by-case basis, individualized in consultation with your physician. Factors such as symptoms, desire to have children, and other pertinent considerations underscore the necessity of tailored decision-making.
Short and to the point
Endometriosis can affect both pelvic and non-pelvic regions. Pelvic wall involvement can lead to additional non-specific symptoms alongside specific complaints like painful menstruation and infertility. Back or leg pain may arise due to lesions affecting sensitive structures such as nerves.
When pelvic wall adhesions are suspected, diagnosis entails discussions, palpation, imaging, and possibly abdominal endoscopy.
Surgical intervention may be warranted depending on severity, with an experienced surgeon crucial due to pelvic sensitivity. Hormone treatments might follow, guided by your doctor’s counsel.
References
- Diedrich, Klaus. Gynecology and obstetrics (Springer textbook) (German Edition) (p.300). Springer Berlin Heidelberg. Kindle version.
- German Society of Gynecology and Obstetrics: guideline program. Diagnosis and therapy of endometriosis. August 2020.
- Endometriose-Vereinigung Deutschland e.V.: Endometriosis rarely comes alone.
- Prof. Dr. med. Marc Possover: Endometriosis – clinic and therapy.
- Nilufer R et al. Large-scale genome-wide association meta-analysis of endometriosis reveals 13 novel loci and genetically associated comorbidity with other pain conditions. bioRxiv. 2018:406967.
- Hauth EA, Stattaus J, Kimmig R, Schmidt M, Forsting M. Magnetic resonance imaging (MRI) of the pelvis in diagnosing endometriosis — a review paper [Magnetic resonance imaging (MRI) of the pelvis in diagnosing endometriosis]. Zentralbl Gynakol. 2005 Apr;127(2):76-82. English. doi: 10.1055/s-2005-836326. PMID: 15800838.
- Gentle diagnosis of endometriosis – MRI detects mucosal islands | DRG.de.
- Investigations for endometriosis | healthinformation.org.
Chen I, Veth VB, Choudhry AJ, Murji A, Zakhari A, Black AY, Agarpao C, Maas JW. Pre- and postsurgical medical therapy for endometriosis surgery. Cochrane - Database Syst Rev. 2020 Nov 18;11(11):CD003678. doi: 10.1002/14651858.CD003678.pub3. PMID: 33206374; PMCID: PMC8127059.
Have you been diagnosed with pelvic wall endometriosis? How did you become aware of it?
Please feel free to leave us a comment.
- Pharmaceutical Companies and Their Influence on Scientific Research - 7. October 2023
- Identification of a Genetic Factor Linked to Endometriosis Development and Potential Therapeutic Targets - 6. October 2023
- Identification of a Genetic Factor Linked to Endometriosis Development and Potential Therapeutic Targets - 6. October 2023