Endometriosis on the Bladder: Symptoms and Therapy
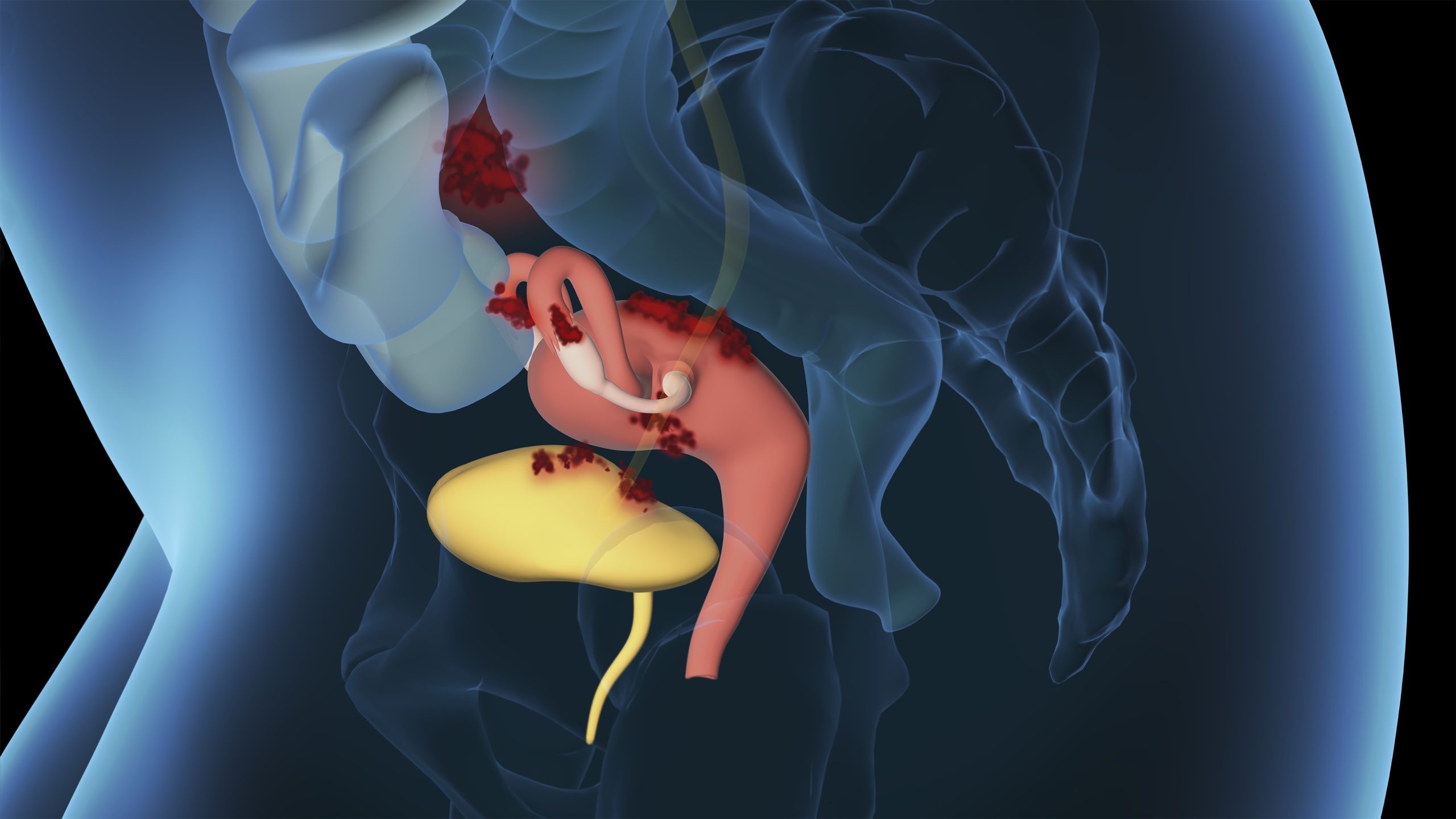
Endometriosis involves tissue similar to endometrium growing outside the uterus. Pathologically or histologically, the tissue that grows in undesired locations is benign. Nonetheless, the various patterns of infestation can result in supplementary symptoms. This applies to endometriosis extragenitalis (endometriosis outside the genital organs). In this scenario, physicians can identify tissue with cells resembling the uterine lining in the bladder, among other sites. [1] Today, I will discuss symptoms, diagnosis, and treatment for endometriosis involving the bladder.
Frequency of Endometriosis with Bladder Involvement
Endometriosis has the characteristic of spreading, with tissue resembling uterine lining colonizing other organs. While it mainly affects the abdomen, pelvic cavity, ovaries, and fallopian tubes, it can settle anywhere in the female body. [2] This includes the urinary bladder, as endometriosis of the urinary tract (urinary tract endometriosis – UTE) occurs in about 1-2% of endometriosis patients, which translates to about two out of 100 individuals with endometriosis experiencing this condition. Doctors distinguish whether the bladder or the ureter is affected in urinary tract endometriosis, with growths commonly seen in women with what is known as deep infiltrating endometriosis (TIE). [3]
Good to know!
A distinguishing characteristic of deep infiltrating endometriosis is that the abnormal tissue not only settles superficially but also grows deeply into the organs. [4]
Endometriosis on the Bladder: Symptoms
Bladder endometriosis presents with non-specific symptoms, making it challenging to use them as a definitive guide for a diagnosis.
The following symptoms may be experienced in cases of bladder endometriosis:
- Pain in the lower abdomen
- Frequent urination with small amounts being excreted
- Urge to urinate
- Painful urination
- Pain when filling the bladder
- Admixtures of blood in the urine (though not always visible to the naked eye and present in only about 20% of cases)
These symptoms bear resemblance to those commonly associated with a urinary tract infection, often leading to misdiagnosis and subsequent initial treatment with antibiotics. [5]
Interstitial Cystitis and Endometriosis – Fraternal Problem Makers
Interstitial cystitis is a chronic non-contagious bladder condition. [6] Unlike typical bladder infections caused by bacteria or pathogens, interstitial cystitis is not linked to such agents. It is estimated that approximately every second to third woman with endometriosis also experiences interstitial cystitis. However, this condition is often diagnosed late because its symptoms can overlap with those of endometriosis. Therefore, a thorough and careful diagnosis is crucial to differentiate and address both contributing issues independently. [7,8]
Diagnosing Endometriosis with Bladder Involvement
If there is suspicion of endometriosis with bladder involvement during doctor-patient discussions (anamnesis), further examinations are conducted to confirm the diagnosis. An essential initial step is an ultrasound, which allows the assessment of the bladder wall non-invasively. Large and medium-sized growths can be easily visualized through ultrasound. However, if the bladder endometriosis measures less than one centimeter in diameter, a magnetic resonance examination may be preferred. Nevertheless, it is important to note that endometriosis on the bladder may not always be visible in these imaging tests, and a negative result does not rule out the condition entirely. When concrete evidence suggests bladder involvement, a cystoscopy is performed, followed by a laparoscopy if necessary. Cystoscopy is instrumental in confirming the diagnosis from inside the bladder. Additionally, this examination can determine if the endometrium affects the orifices of the ureters or if other factors contribute to the pain. [5] It is important to recognize that endometriosis is frequently found on the outside of the bladder, growing from the abdomen onto the bladder’s surface. Consequently, it may not be visible from the inside during an endoscopy. Therefore, an inconspicuous cystoscopy does not definitely rule out bladder involvement. In such cases, laparoscopy is employed to locate and remove the endometrial foci on the external side of the bladder. This procedure also allows assessment of the remaining course of the ureters.
Good to know!
If cystoscopy does not reveal endometriosis with bladder involvement, it is still common practice to take tissue samples from the bladder wall. These are later examined in the laboratory to rule out the possibility of interstitial cystitis. [5]
Therapy for Endometriosis on the Bladder
In everyday clinical practice, surgical intervention takes precedence over drug treatment for endometriosis in the bladder. For cases where endometriosis growth is superficial, a procedure called “shaving” can be performed, where the endometriosis is removed from the bladder’s surface. However, the most promising treatment option is a partial cystectomy, which involves removing the infiltrating tissue and the affected portion of the bladder. Patients often report a decrease in pain following this procedure. The thorough removal of endometriosis during the cystectomy leads to a lower recurrence rate, reducing the risk of endometriosis returning to the bladder compared to other methods. Minimally invasive techniques, involving small incisions, are commonly used for partial cystectomy. After the procedure, an indwelling catheter is usually placed for approximately 5–10 days. Before removal, a leakage test is conducted by medical professionals to ensure the bladder is functioning properly. [3,5]
Good to know!
Available studies indicate that the recurrence rate with partial bladder removal for endometriosis is relatively low, ranging from about 0-16%. Moreover, a significant improvement in symptoms is reported in 85-100% of cases following the procedure. [3]
However, it’s essential to recognize that no surgery is entirely risk-free. Therefore, before undergoing any procedure, a detailed discussion with the medical team is crucial, especially when considering the possibility of bladder involvement due to endometriosis. Often, the extent of endometriosis cannot be accurately determined before the surgery, leading to the need to discuss “what if …” scenarios. So what are the recommended steps for managing bladder involvement in endometriosis?
If a portion of the bladder needs to be removed for complete endometriosis removal, specific considerations come into play. For instance, a bladder catheter may be inserted for about 10 days, or possibly longer (depending on the procedure’s size) to ensure the bladder remains empty and heals properly. These and other particulars should be discussed during the informed consent interview. This way, you can decide whether you prefer certain aspects of the operation, such as surgery on the bowel or bladder, to be performed directly to achieve complete endometriosis removal. Alternatively, you may choose to discuss the options again in such cases to have a better understanding of what to expect, even if it means the possibility of a second operation if needed.
In a Nutshell
In summary, endometriosis involves the infiltration of endometrial-like tissue into organs, leading to deep infiltrating endometriosis, which often affects the bladder in diagnosed women. This can result in non-specific symptoms such as lower abdominal pain, urinary urgency, and painful bladder emptying, resembling those seen in urinary tract infections or interstitial cystitis. Interstitial cystitis, a chronic bladder infection, is frequently found in patients with endometriosis. When the bladder is involved, a careful diagnosis through ultrasound and cystoscopy is crucial, and medication is not the primary treatment approach. Instead, therapy often entails the removal of part of the bladder and affected tissue. The final treatment choice is individualized, taking into account specific symptoms and findings.
Would you like to learn more about endometriosis of the bladder or other symptoms? Then download the Endo-App and benefit from the knowledge of our experts.
References
- Endometriosis (deutsche-apotheker-zeitung.de)
- Endometriosis ” (frauenaerzte-im-netz.de)
- pdf (endometriosis-sef.de)
- Heidelberg University Hospital: Endometriosis (uni-heidelberg.de)
- 015/045 – Diagnostics and therapy of endometriosis (awmf.org)
- Interstitial Cystitis – Kidney and Urinary Tract Diseases – MSD Manual Issue for Patients (msdmanuals.com)
- Chronic inflammation often affects multiple organs – BGV Info Health (bgv-info-gesundheit.de).
- Wu CC, Chung SD, Lin HC. Endometriosis increased the risk of bladder pain syndrome/interstitial cystitis: A population-based study. Neurourol Urodyn. 2018 Apr;37(4):1413-1418. doi: 10.1002/nau.23462. epub 2018 Jan 10. PMID: 29318645.
- Pharmaceutical Companies and Their Influence on Scientific Research - 7. October 2023
- Identification of a Genetic Factor Linked to Endometriosis Development and Potential Therapeutic Targets - 6. October 2023
- Identification of a Genetic Factor Linked to Endometriosis Development and Potential Therapeutic Targets - 6. October 2023